Rheumatoid Arthritis & Diet
This Food Fact Sheet is about the role that diet may have in managing symptoms of rheumatoid arthritis. Arthritis literally means the inflammation of joints.
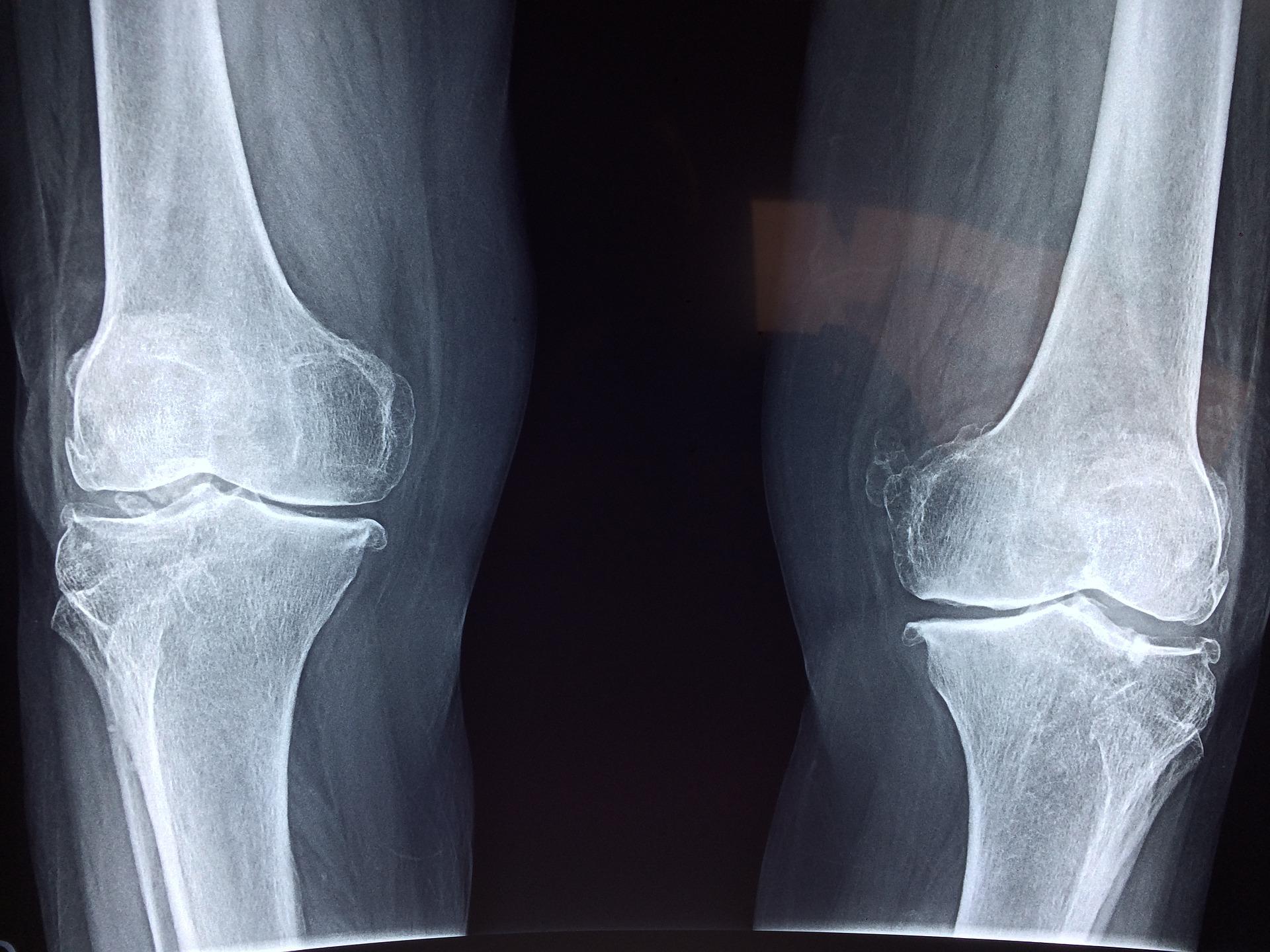
What is rheumatoid arthritis (RA)?
RA is a systemic autoimmune condition that can affect organs such as the eyes, lungs, heart as well as synovial (movement) joints. The most affected are the small joints in the hands and feet but it can affect knees, hips and shoulder joints too. Several joints can be affected at the same time, usually symmetrically (on both sides of the body), such as both hands. RA causes the joint lining to become inflamed and swollen. This results in destruction of the joint surface, causing extreme tenderness and pain. Increased inflammation in people who have RA increases the risk of developing heart attack, stroke, and heart failure.
Who is affected?
RA affects around 1% of the UK population aged 16 and over. This translates to about 400,000 people living with this condition. It is worth noting that this disease is two to four times more common in women than men. The onset of this disease can occur at any age but peaks at ages 30-60.
Treatment
Rheumatologists are experts in joint diseases. They work with a team of health professionals including specialist nurses, physiotherapists, occupational therapists, pharmacists, podiatrists and sometimes dietitians who give advice on medications, pain management, exercises to improve joint function and diet.
Up to 75% of people living with RA believe diet plays a key part in their symptoms. Published data found 50% of people have tried to alter their diet. Available evidence does not support dietary change as a substitute for medication but you may find these tips helpful.
Stay a healthy weight
The most important relationship between diet and arthritis is weight. Excess weight can make some specialist medications ineffective. It may increase disease activity and delay remission. If you are carrying more body weight than you should, try and lose the excess weight by combining healthy eating with regular exercise.
Change the type of fat in your diet
People with RA have a higher risk of developing heart disease than those who don’t have the disease. The amount and type of fat you eat and use in cooking may influence blood cholesterol levels, and might also influence the level of joint pain and inflammation. Reducing your intake of saturated fat and replacing it with a smaller amount of unsaturated fats may help to maintain normal blood cholesterol levels.
Watch out for overall high salt intake
Salt (sodium chloride) intake above 6g per day may promote inflammation due to changes in the immune system. A high salt intake can also increase the risk of high blood pressure for some individuals.
Eat more oily fish or consider having fish oil
Fish such as sardines, mackerel, herring, fresh tuna, salmon, and snapper have darker flesh which is rich in omega-3 polyunsaturated fats. In addition to their heart health benefits, fish oils have been shown to help dampen general inflammation and may help to reduce joint pain and stiffness.
Try to eat two portions (one portion = 140g or a small fillet) of oily fish a week. Some eggs and breads are enriched with omega-3. Omega-3 fats from plant sources (GLA) such as linseed, evening primrose and borage oils have a weaker effect on reducing inflammation and are of limited benefit.
High-dose fish oil supplements have been shown to reduce symptoms of RA, such as the duration of morning stiffness, the number of swollen and tender joints and joint pain. Fish oil supplements should have 500-1000mg of EPA and DHA (omega-3 fats) per capsule. Be patient, as it can take up to three months for symptom relief. Speak to your doctor before taking any new supplements.
‘Mediterranean-style’ diet
There is no specific diet for arthritis. A healthy varied diet is recommended. There has been a lot of interest in the Mediterranean diet. This diet includes poultry, fish, and small quantities of lean red meat as well as plenty of vegetables and fresh fruit (fresh, frozen or canned), plenty of olive oil, wholegrain cereals, peas, beans, nuts and seeds. This means saturated fats are reduced and replaced by unsaturated fats including omega-3 fats.
Research is inconclusive but some studies have shown an improvement in the symptoms experienced by people with RA when following this diet.
To adopt this way of eating, aim for four or more portions of vegetables and two or more portions of fruit daily. Use more oils and products rich in monounsaturated fats such as olive and rapeseed oil. Eating an assortment of colourful fruits and vegetables (5-a-day) will increase your intake of compounds called ‘antioxidants’ which may help to reduce inflammation.
Eat iron-rich foods
Anaemia is a deficiency of red blood cells to transport oxygen around the body. Anaemia can be caused by chronic inflammation, medications and impaired iron absorption. Therefore adequate dietary intake of iron is important to help prevent fatigue. Tiredness is a very common symptom of RA and can be made worse by anaemia.
To try to help tackle this, do not avoid lean red meat completely, even if you are following the Mediterranean diet. Iron is more easily absorbed by the body if you have it at the same time as vitamin C, so have a portion of fruit or a small glass of fruit juice with your meals. If you are following a plant-based diet, our Iron fact sheet explains where you can get iron from.
Eat calcium-rich foods
It is important that everyone gets enough calcium in their diet to ensure that their bones stay strong and healthy. This is an even greater consideration when you have RA and are using glucocorticoids as part of the treatment. It may put you at a higher risk of developing osteoporosis as well as weight gain. Good sources of calcium include low fat milk, yoghurt and cheese, green leafy vegetables, soya drinks with added calcium, almonds and fish where you eat the bones, such as sardines and pilchards.
Exclusion diets and food intolerance
A vegetarian diet may help relieve symptoms for some. Speak to your doctor or dietitian to make sure you are still getting enough nutrients. Some people believe that a food allergy or intolerance causes or exacerbates inflammation in RA, but there is no evidence to support this theory. However, a small number of people with RA may have a genuine intolerance to one or more foods. Offending foods can be identified through an exclusion programme under the supervision of a dietitian. Fasting is an extreme and temporary way of controlling pain and inflammation in RA and is not recommended.
Supplements
Vitamin D
There may be an association between low vitamin D levels and RA. All adults and children over the age of one should consider taking a daily supplement containing ten micrograms of Vitamin D especially during autumn and winter in the UK. Those in the at risk groups, should consider taking a supplement containing ten micrograms of Vitamin D all year round.
Antioxidant vitamins or mineral supplements
There is no scientific evidence to support the use of antioxidant vitamins or mineral supplements in the treatment of RA. A healthy diet contains all the nutrients needed by the body. However, if your diet is very restricted or your appetite is poor, a general multivitamin or mineral supplement may be beneficial. Speak to your doctor before taking a new supplement.
Gut bacteria and RA
It is established that the gut microbiome plays a role in immune system regulation. Emerging research suggests that changes to gut bacteria may be associated with an increased risk of RA. People with RA have been observed to have irregular gut bacteria but so far, the use of probiotics as a treatment has not been proved to be effective.
Top tips
- Diet alone can't reduce disease activity, but many with RA believe diet plays a key part in their symptoms
- It is important to maintain a healthy weight. Healthy eating combined with regular exercise will assist in the loss of body fat
- Carrying extra body weight increases the risk of cardiovascular disease. It also impairs the efficacy of some specialist anti-rheumatic medications such as biologics
- Reduce the amount of saturated fat and eat more omega-3 and monounsaturated fats (such as olive oil) to benefit your joint and heart health
- Nutrients such as iron, calcium and vitamin D are very important
- Following a ‘Mediterranean style’ diet may improve your symptoms
- A lower salt (sodium chloride) diet may also be beneficial
- Discuss any changes in your diet with your rheumatologist and dietitian