Managing Your Symptoms
When your symptoms get worse, this is known as a flare-up. These can happen at any time, but can happen after you have been stressed or had an infection. Over time, you may get better at noticing the early signs of a flare-up. If you’re having regular flare-ups, you should mention this to your doctor. It may be that you need to review your treatment.
Here are a few things you can do to help yourself during a flare-up:
- Keep taking your medication at the doses you’ve been prescribed.
- Do gentle exercises.
- Put heated items on the joint – these can include a hot water bottle or electric heat pad. See below for more information.
- Put cold items on the joint – these can include a bowl of cold water with ice cubes, a pack of frozen peas wrapped in a towel, or a damp towel that has been kept in the fridge. See below for more information.
- Let people around you know, so they can help and support you.
Tips for using heated items
Heated items that could help your joint pain include a hot water bottle or electric heat pad. Wrap these in a towel, then place on a painful joint. You could also try having a hot or warm shower or bath. Make sure these items are warm but not hot, as you could risk burning or scalding yourself. Gentle heat will be enough.
A towel should be placed between the heated item and the skin for protection. Check your skin regularly, to make sure it is not burning.
Tips for using ice packs
Some people find that using an ice pack can help their joint pain. You can buy one from a pharmacy, or you can make one at home, by wrapping ice cubes in a plastic bag or wet tea towel. Here’s how to apply the ice to your skin:
- Rub a small amount of oil over where you’d like the ice pack to go. Any type of oil can be used. If your skin is broken – for example, if you have a cut – don’t use the oil and cover the area with a plastic bag. This will stop the cut getting wet.
- Put a cold, wet flannel over the oil.
- Put the ice pack over the flannel and hold it there.
- After five minutes, check the colour of your skin. Remove the ice pack if your skin has turned bright pink or red. If it hasn’t, leave it on for another 5 to 10 minutes.
- You can leave the ice pack on for 20-30 minutes. Don’t leave it on for any longer, as you could damage your skin if it is left on for too long.
Physical activity
Keeping physically active can improve your rheumatoid arthritis symptoms, including pain. You may find it difficult to be physically active in the first place, especially if you are having a flare-up. However, if you find the right activities, help and support, you can be active in a way that suits you.
Not keeping active can lead to stiff joints and weak muscles. It could also cause you to gain weight. However, if a type of exercise always causes a flare-up, it's probably best to find another one. High-impact exercises such as step exercises, or contact sports, such as rugby and football, are more likely to cause problems. Swimming, walking, gentle cycling and aqua aerobics generally put less strain on your joints.
Yoga and tai chi are generally thought to be suitable for those with rheumatoid arthritis. However, there are many different styles, so it is best to check the style is suitable for your condition before you sign up to a class.
Physiotherapy
A physiotherapist can suggest suitable exercises for you and support you in keeping active. People with rheumatoid arthritis should have access to specialist physiotherapy to help manage their condition and improve their fitness, flexibility and strength. You should also have follow-up reviews.
Hydrotherapy
You may also find that hydrotherapy helps to ease your symptoms. This involves doing special exercises in a warm-water pool, under the supervision of a trained physiotherapist. Hydrotherapy can also be called ‘aquatic therapy’ or ‘aquatic physiotherapy’.
Check with your GP or call your local rheumatology department to find out if an NHS physiotherapist in your area will accept self-referrals.
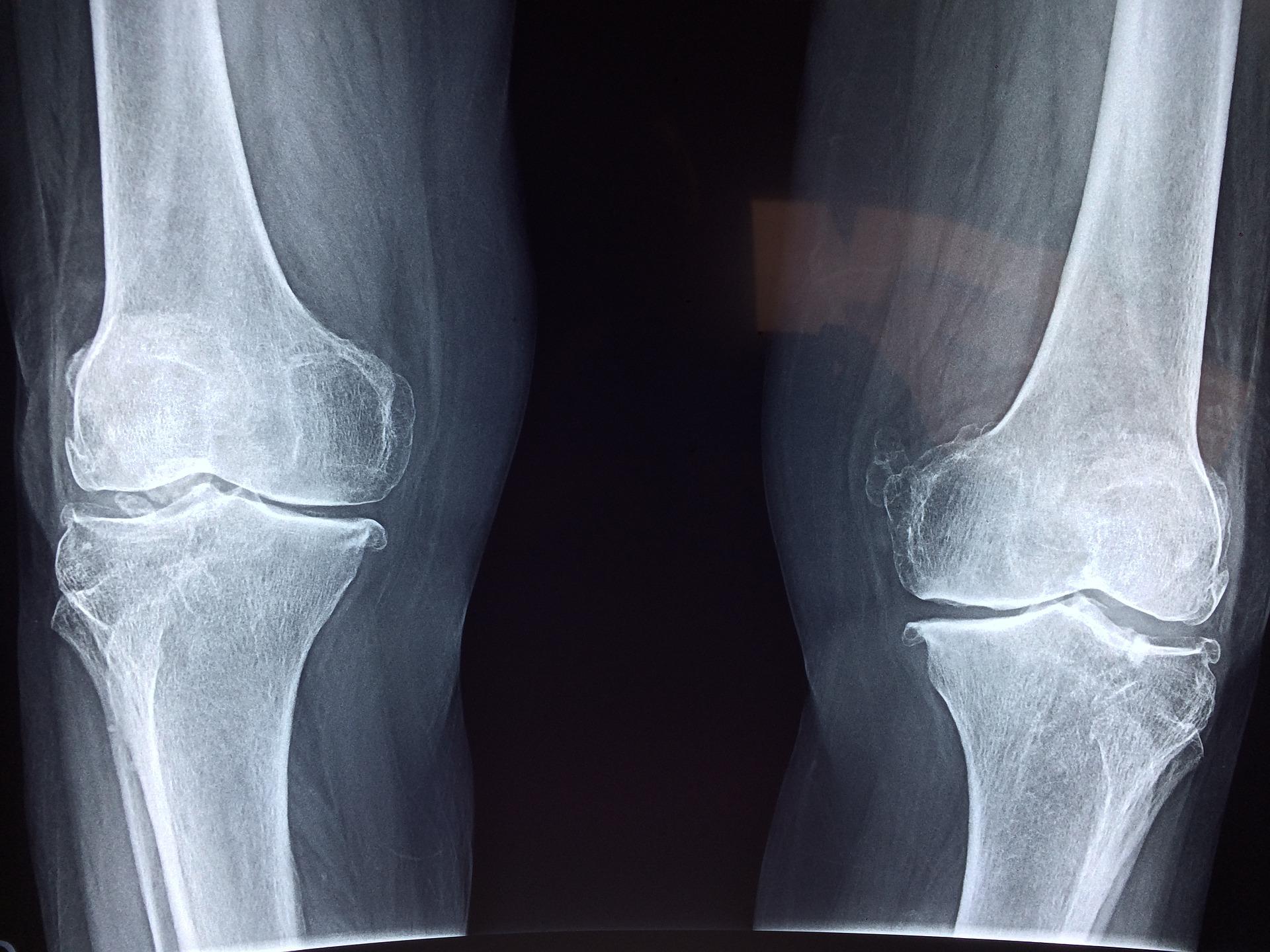
Foot problems
Foot problems for those with rheumatoid arthritis include:
- pain
- soreness
- warmth and swelling that lasts at least a few days
- the foot changing shape
- difficulty walking
- your shoes rubbing
- corns or calluses, and nail problems
- Infections such as athletes foot, verruca or bacterial infections.
If these problems are left untreated, they can lead to the infections spreading and, eventually, to ulcers forming. It is therefore important to see a podiatrist, who specialises in general foot care. They can give advice on footwear, information on how to treat foot problems yourself, and can provide special insoles. They can also monitor your foot and general health, and will refer you to a consultant if they find any issues.
Complementary treatments
Complementary treatments can be useful when used alongside prescribed medicines for the treatment of rheumatoid arthritis. However, they should not replace your prescribed medicines and you should talk to your rheumatology team before starting a complementary treatment.
Generally complementary treatments aren't considered to be evidence-based and are therefore not usually available on the NHS.