Diet & Rheumatoid Arthritis
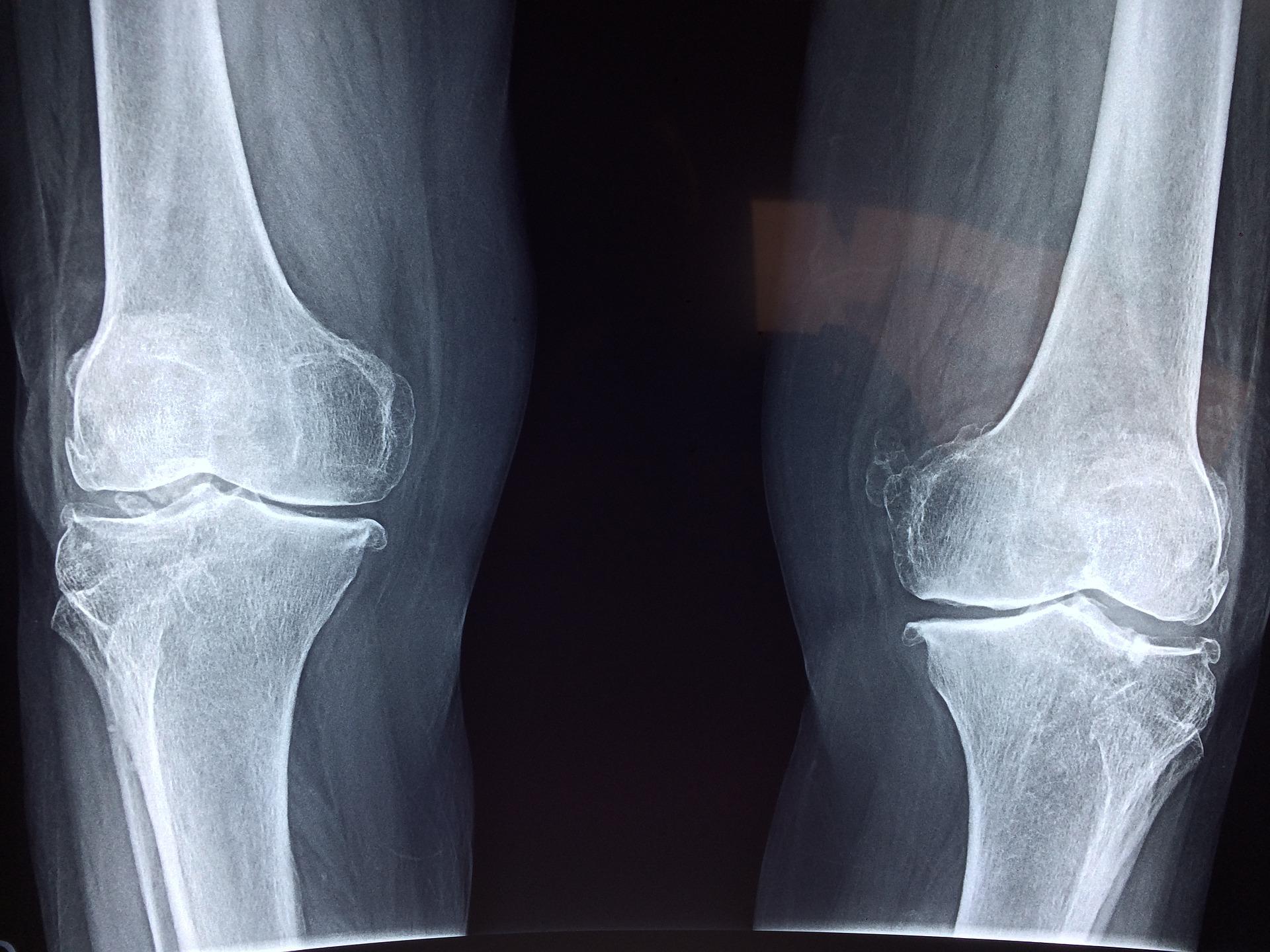
Rheumatoid arthritis (RA) is a long-term inflammatory condition that causes pain, swelling and stiffness in joints. The hands, wrists and feet are typically affected, but it may affect almost any joint. It is an auto-immune condition so happens when the body’s immune system, which usually fights infection, starts to attack healthy joints instead. At times symptoms can become suddenly worse causing severe pain and making it hard to go about normal everyday life. Rheumatoid arthritis is associated with a number of complications and comorbidities (conditions that often occur together with another condition) such as an increased risk of cardiovascular disease and osteoporosis (a condition that weakens bones).
Rheumatoid arthritis is less common than osteoarthritis, but it nonetheless is estimated to affect over 400,000 adults in the UK. There is no permanent cure, and it can have a significant personal impact for people with the disease and their families and carers. However, early treatment can help to control it and help people carry on active and full lives. Medical management with drug therapy aims to relieve pain and stiffness and help mobility, and to change the progress of the disease that can limit functioning in daily activities.
Rheumatoid arthritis and diet
Diet and inflammation
People living with RA often use dietary changes and follow a variety of special diets to try to improve symptoms. A wide range of anecdotal dietary advice is available to improve symptoms but there is a lack of scientific information to support these, and some of the claimed benefits for diets are yet to be confirmed.
The most common dietary patterns tried are those that may have anti-inflammatory benefit or increase antioxidant levels (see section on antioxidants below). Other dietary strategies focus on cutting out foods or food groups that may be perceived as the cause of symptoms. Diets often tried include vegan, Mediterranean, elemental or elimination diets. However, much clarification is still needed to understand the relationship between diet and RA. It is currently unclear from the research whether diets can improve pain, stiffness and the ability to move better. Available evidence does not establish diet as a substitute for pharmaceutical treatments.
For people living with RA it is important to be aware of the dietary advice for which there is some evidence of benefit, and where the evidence is limited, as well as awareness that some alternative diets proposed can compromise nutrient intake.
What does the research say?
Mediterranean diet
UK NICE guidelines recommend that adults with RA who wish to experiment with their diet should be informed that there is no strong evidence that their arthritis will benefit. However, they could be encouraged to follow the principles of a Mediterranean diet. The Mediterranean diet is rich in plant-based foods such as wholegrains, beans, pulses, fruit and vegetables, and with moderate amounts of fish, low to moderate amounts of dairy products, low intake of meat, and olive oil as an important fat source.
Whilst research supports the Mediterranean diet for certain conditions such as the prevention of cardiovascular disease, there is limited evidence currently to suggest that the Mediterranean diet is beneficial in the prevention and treatment of RA.
Rheumatoid arthritis and supplements
Antioxidants
A diet rich in antioxidants may help to reduce the risk of developing RA and possibly dampen down the inflammatory response in established disease. These nutrients can be found in a healthy, balanced diet (see table below for dietary sources). However, the benefit of antioxidant nutrient supplements like vitamin A, vitamin C, vitamin E, selenium and zinc is not supported by scientific trials in patients with RA. In addition, it is important to note that ‘mega-dosing’ (intakes in doses well above current recommendations), whether self-administered or suggested by alternative practitioners, can have adverse effects and is inadvisable.
Fish oils
There is some evidence to suggest that taking fish oil supplements may be useful as an addition to existing treatments for reducing joint pain and stiffness.
The long-chain omega-3 fats found in fish oils, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), are reported to have anti-inflammatory properties. Reviews and meta-analyses of studies that have explored benefit of fish oil and long-chain omega-3 fats in RA have had inconsistent findings. Some studies show that long-chain omega-3 fats may help to reduce joint swelling and pain, morning stiffness, in addition to reducing the amounts of medication for symptom relief that patients need. Other studies have found that they do not significantly affect the clinical symptoms of RA.
Whilst the current UK NICE guidelines for management of RA do not discuss the role of fish oil supplements, their use of appears to be common among RA patients. However, the optimal dose of long-chain omega-3 fats that may be helpful in relieving symptoms of RA is unclear, and it has been reported that supplementation can take up to three months before symptom relief is experienced.
Whilst there is not enough evidence to routinely recommend omega-3 supplements eating at least one portion of oily fish is included in dietary advice for the general population. Oily fish (such as mackerel, sardines and salmon) are the best source of these fatty acids in our diets and contain other nutrients such as vitamin D. Therefore, fish consumption is promoted in patients with RA, in line with general healthy eating recommendations (which is to eat at least two portions of fish each week, at least one of which should be oily fish; note pregnant women should not eat more than two portions of oily fish a week).
Probiotics
More recently, scientists have suggested that the gut microbiome – the bacteria that live in our gut – may also be a factor in the development of RA but the clinical effects of probiotics (usually described as ‘good’ bacteria found in food products/supplements) in RA remain unclear.
Elimination diets and fasting
Eliminating foods
It is a common belief among people living with RA that certain foods or ingredients have adverse effects, and that a food allergy/intolerance may cause or make inflammation worse. Several reviews have aimed to evaluate the effectiveness of a range of interventions that restrict certain foods for the treatment of RA and management of its side effects. These include:
- vegan diets
- elemental diets (liquid diets that contain nutrients that are broken down to make digestion easier)
- fasting
- elimination diets (used to find foods that might be the cause of symptoms)
However, there is very limited research in this area and the results remain largely unclear. It is uncertain whether any of these dietary strategies can improve pain and stiffness, and the ability to move better. There may be considerable individual variation, in other words, certain individuals or subgroups may show improvement if they cut out certain foods or ingredients, but many others do not. Furthermore, some of these diets may be difficult to stick to, and people may lose weight on these diets even though they did not need or plan to.
There is no test that currently can identify an individual RA patient that may experience benefit by a change in diet, although offending foods can be identified through an exclusion programme under the supervision of a dietitian, if appropriate.
Fasting
Reduction of pain and inflammation has been reported with fasting and elemental diets. It is recognised that inflammatory activity is dampened by caloric restriction or reduction in gut involvement, but the results noted after fasting and very restricted diets could also be because of weight loss. In addition, such diets are not sustainable and carry significant health risks. Fasting is an extreme and temporary way of controlling pain and inflammation in RA and is not recommended. Symptoms return on resumption of regular diets; thus the benefit may be transient and not have long-term impact on disease activity.
A quick look at milk and dairy foods
There has been some suggestion that dairy foods are associated with inflammation, but the evidence is conflicting, and limited to small trials.
In the past dairy may have been considered pro-inflammatory, but more recent reviews of the evidence do not support this hypothesis. Studies of milk and dairy products more typically suggest a neutral or even beneficial effect on levels of inflammatory markers and would not point to an adverse inflammatory effect.
Specific dietary guidelines are difficult to define in people living with RA as there are individual differences. However, as dairy products can play an important part of a healthy, balanced diet, based on the available data, there is no evidence to support exclusion of dairy products unless an intolerance or allergy are shown. If you think you may have an adverse reaction to milk and dairy products talk to your GP or a health professional involved in your care such as your specialist nurse.