Diet & Osteoarthritis
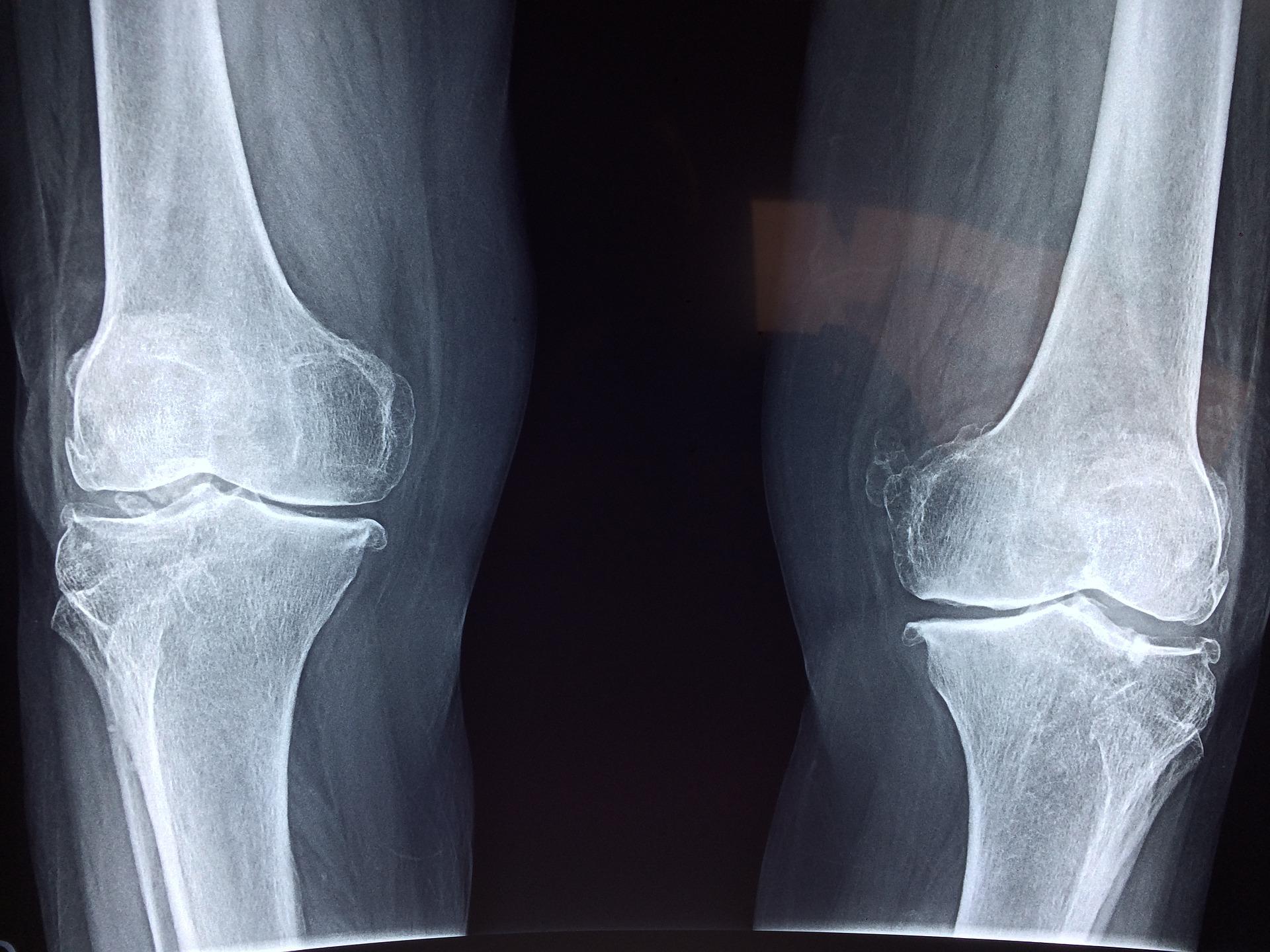
Osteoarthritis (OA) is the most common type of arthritis in the UK, affecting nearly 9 million people. It is a disease that damages the cartilage, the tissue that cushions joints and helps them move smoothly, making movement harder and leading to increased stiffness and pain.
Osteoarthritis can affect any joint in the body, but the most common areas affected are the knees, hips and small joints in the hands. The management of OA focuses on symptom management. It is not possible for specific foods or nutritional supplements to cure osteoarthritis, but diet and exercise can be important to help ease symptoms.
It is widely accepted that weight reduction (if overweight) in combination with increased physical activity can improve function and symptoms such as pain and stiffness and should form part of the treatment for OA.
Osteoarthritis and diet
A healthy weight
Weight loss is recommended as a core treatment for people who are overweight and obese. Reaching or maintaining a healthy weight can relieve pain, improve function, and slow the progression of OA.
Overweight is a crucial factor in OA since overload to the affected joint is one of the risk factors for developing OA or worsening of the symptoms of OA. Losing weight reduces pressure on joints, particularly weight bearing joints like the hips and knees.
There is increasing interest in not only reducing weight but specifically in reducing fat (or adipose) tissue, as it is now recognised that fat tissue is active and can secrete several chemical factors, some of which may have inflammatory effects.
Osteoarthritis and physical activity
Painful joints and stiffness can reduce mobility and make it more difficult to be physically active. However, physical activity can help maintain a healthy bodyweight and protect joints by keeping muscles strong, reduce joint loading, increasing your range of movement and reducing stiffness.
Local muscle strengthening exercises (activities such as yoga, pilates or dancing that work the major muscles) and aerobic exercise (activities such as walking, cycling or swimming that temporarily increase your heart rate and respiration) are recommended.
It is important to find the right type of activity for you. Ask your GP to refer you to a physiotherapist, who can help you work out a suitable programme.
Should I take supplements for osteoarthritis?
Many people with OA report trying various dietary supplements to relieve pain and improve function.
Glucosamine and chondroitin sulphate
Joint cartilage normally contains glucosamine and chondroitin compounds, and it’s thought that taking these as supplements, which are often available in combination, may help to improve the health of damaged cartilage. However, although these supplements are considered to be safe, evidence of clinical benefit is minimal, and prescribing of supplements such as glucosamine and chondroitin is not routinely recommended for the management of OA.
If you do decide to take glucosamine and/or chondroitin, always seek advice from your pharmacist on potential interactions with other medications you may be taking. For glucosamine doses usually indicated are between 1250 and 1500mg per day, with a review of treatment if no benefit is noticed after 2–3 months. Note: these supplements are often made from shellfish, and so are not suitable if you have a shellfish allergy.
For chondroitin there is no established dose for OA, but manufacturers tend to recommend between 400 and 1200mg daily.
Vitamin D
Vitamin D is important for building and maintaining overall bone health. Although some research has suggested an association between low levels of vitamin D and increased risk and progression of OA, trials do not support vitamin D supplements for easing OA pain and joint degeneration. Nonetheless people with OA should follow government advice for the general population to consider taking a daily supplement containing 10µg (micrograms) of vitamin D during the autumn and winter months when the sun is not strong enough for the body to make vitamin D.
Other supplements like turmeric and fish oils
There is generally very limited, conflicting and poor-quality evidence on dietary supplements and complementary treatments such as MSM (methylsulfonylmethane), rosehip and curcumin (the active ingredient in turmeric) supplements used by people living with OA for symptomatic relief. Further research is needed to understand whether any supplement may be of benefit and be safe.
In addition, there is no strong evidence as yet that fish oil supplements can confer any benefit for OA but including oily fish in your diet is recommended (at least two portions of fish a week, including one of oily fish*), in healthy eating advice for the general population.
*Note: Pregnant women should not eat more than two portions of oily fish a week.
Healthy dietary patterns for osteoarthritis and more
Some research suggests a link between high blood cholesterol and increased risk and progression of OA, although it is unclear whether lowering blood cholesterol will improve OA. In any case raised blood cholesterol is a risk factor for cardiovascular disease and it is important to try and adopt healthy dietary patterns that may help to reduce blood cholesterol and the risk of cardiovascular disease, and maintain weight – see some of our tips below.
- Try to include a variety of at least five portions of fruit and vegetables, higher fibre starchy foods (choose wholegrain or higher fibre versions with less added fat, salt and sugar), dairy and dairy alternatives (choose lower fat and lower sugar options), as well as beans, pulses, fish, eggs, lean meat and other protein sources. Avoid unhealthy habits, like smoking and drinking in excess and include regular physical activity.
- A healthy diet includes plenty of foods containing fibre such as nuts, wholegrains, beans, pulses, fruits and vegetables. But for cholesterol lowering you may want to also try eating oats and barley, which have a special soluble fibre called beta–glucan which can help to reduce blood cholesterol levels.
- Reduce foods high in saturated fats in your diet like sausages, butter, biscuits, cake, pies, pastries and fatty meats, and replace with those containing unsaturated fats (mono- and polyunsaturated), like oily fish, avocados, nuts and seeds and small amounts of olive, rapeseed and sunflower oils and unsaturated spreads made from them (see image below).