Causes & Symptoms
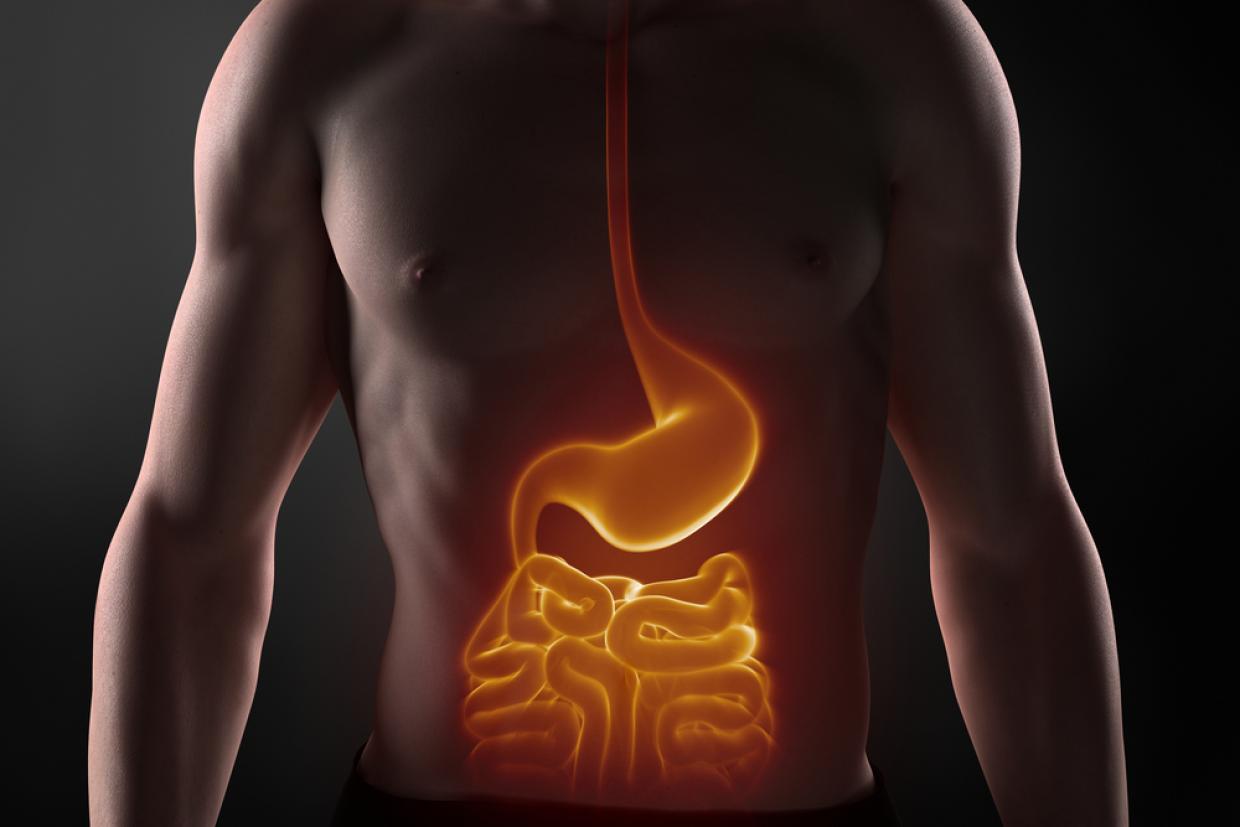
Diverticular disease is caused by small bulges in the large intestine (diverticula) developing and becoming inflamed. If any of the diverticula become infected, this leads to symptoms of diverticulitis.
The exact reason why diverticula develop is not known, but they are associated with not eating enough fibre. Fibre makes your stools softer and larger, so less pressure is needed by your large intestine to push them out of your body.
The pressure of moving hard, small pieces of stools through your large intestine creates weak spots in the outside layer of muscle. This allows the inner layer (mucosa) to squeeze through these weak spots, creating the diverticula.
There is currently no clinical evidence to fully prove the link between fibre and diverticula. However, diverticular disease and diverticulitis are both much more common in Western countries, where many people do not eat enough fibre.
Diverticular disease
It is not known why only 1 in 4 people with diverticula go on to have symptoms of diverticulitis. Diverticular disease may be chronic low-level diverticulitis. The symptoms are very similar to irritable bowel syndrome (IBS) and may overlap. However, factors that appear to increase your risk of developing diverticular disease include:
- smoking
- being overweight or obese
- having a history of constipation
- use of non-steroidal anti-inflammatory drugs (NSAIDs) painkillers, such as ibuprofen or naproxen
- having a close relative with diverticular disease, especially if they developed it under the age of 50
Exactly how these lead to developing diverticular disease is unclear.
Symptoms of diverticular disease and diverticulitis
Symptoms of diverticular disease and diverticulitis include abdominal pain, bloating and a change in normal bowel habits.
Diverticulosis
If diverticula have been discovered during a camera test for another reason (colonoscopy) or during a CT scan, you may be worried about what this means. However, if you have never had abdominal pain or bouts of diarrhoea, there is a 70-80% chance that you will never have any symptoms from them.
Diverticula are extremely common over the age of 70 and they do not increase your risk of cancer. It's thought that a high-fibre diet is likely to reduce the risk of any symptoms developing.
Diverticular disease
The most common symptom of diverticular disease is intermittent (stop-start) pain in your lower abdomen (stomach), usually in the lower left-hand side. The pain is often worse when you are eating, or shortly afterwards. Passing stools and breaking wind (flatulence) may help relieve the pain.
Other long-term symptoms of diverticular disease include:
- a change in your normal bowel habits, such as constipation or diarrhoea, or episodes of constipation that are followed by diarrhoea – a classic pattern is multiple trips to the toilet in the morning to pass stools like "rabbit pellets"
- bloating
Another possible symptom of diverticular disease is bleeding dark purple blood from your rectum (back passage). This usually occurs after diarrhoea-like cramping pain, and often leads to hospital admission, but fortunately this is an uncommon complication.
Diverticular disease does not cause weight loss, so if you are losing weight, seeing blood in your stools or experiencing frequent bowel changes, see your GP.
Diverticulitis
Diverticulitis shares most of the symptoms of diverticular disease (see above). However, the pain associated with diverticulitis is constant and severe, rather than intermittent. It is most likely to occur if you have previously had symptoms of diverticular disease, and develops over a day or 2. Other symptoms of diverticulitis can include:
- a high temperature (fever) of 38C (100.4F) or above
- a general feeling of being tired and unwell
- feeling sick (nausea) or being sick (vomiting)
The pain usually starts below your belly button, before moving to the lower left-hand side of your abdomen. In Asian people, the pain may move to the lower right-hand side of your abdomen. This is because East Asian people tend to develop diverticula in a different part of their colon for genetic reasons.