Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is thought to affect 10% to 20% of the population. It does not cause damage to your bowel but the symptoms can have a dramatic impact on your quality of life.
What are the symptoms of IBS?
Symptoms can vary from person to person and from one day to another. They may also get worse after eating or eating certain foods. The most common symptoms are:
- abdominal pain or discomfort
- constipation and/or diarrhea
- bloating and/or distension, wind
- passing mucous
- nausea
- urgency to open bowels
- incomplete evacuation (a feeling of inability to pass all stool)
What causes IBS?
IBS is a chronic condition, and the specific cause of IBS is not known. There is evidence to suggest that it can be caused and worsened by a combination of factors however genetics, diet, gut bacteria or changes in these bacteria as a result of infection or antibiotics, and stress have been found to play a part in IBS. Studies have also shown that a person who has IBS, has a gut that is 'more in tune' to factors such as food and gas production and their body may experience pain or a change in bowel habit in response to these. Strategies to manage IBS include medication, diet and lifestyle factors and probiotics.
How is IBS diagnosed?
There are no tests to diagnose IBS. However, it is advised that you discuss your symptoms with your GP in order to obtain a diagnosis of IBS or to rule out other digestive conditions such as inflammatory bowel disease or coeliac disease. It is important to inform your GP if you have any of the following:
- Rectal bleeding
- Unintentional and unexplained weight loss
- A family history of bowel or ovarian cancer
- A change in bowel habit to looser and /or more frequent stools persisting for more than six weeks in a person aged over 60 years
If you are having a coeliac test you must include gluten in your diet in more than one meal per day for at least 6 weeks up to the time of the test. Common foods that contain gluten include cereals, bread, pasta and noodles.
What changes reduce symptoms?
Diet and lifestyle changes can help reduce symptoms. The following tips can help:
Eat regular meals
- Include breakfast, lunch, and an evening meal every day.
- If having snacks, ensure you are making healthy choices.
- Avoid missing meals or leaving long gaps between eating.
- Try to take time to sit down and relax at mealtimes. • Eat smaller meals and chew food well.
- Be mindful about correct portion sizes.
- If symptoms are worse at night, avoid eating late.
Eat fruit and vegetables
- Aim to have at least 5 portions of variety of fruit and vegetables spread out throughout the day.
Cut down on high fat foods
- Foods like butter, cream and creamy sauces, cheese, pizza, chips, cakes, biscuits, chocolate, pies, pastries, crisps and fatty meats such as burgers and sausages can make symptoms worse in certain individuals.
- They are also high in saturated fat and should be limited to help you stay healthy and manage your weight.
- Reduce intake of processed foods and cook from fresh ingredients where possible.
Get enough fluid
- Drink 1.5-3L of fluid every day – water, decaffeinated drinks and herbal and fruit teas are good sources.
- Limit caffeine-containing drinks to three cups per day.
- Avoid fizzy drinks as they can often make symptoms worse.
- A good way to ensure you keep hydrated is to check your urine is a pale yellow/straw colour.
Reduce alcohol
- If you find that alcohol is worsening symptoms, consider reducing your intake.
- Keep to recommended limits for alcohol which is 17 units weekly for males and 11 units weekly for females and avoid binge drinking.
- I unit is equal to ½ pint of beer/larger/cider/stout, a 125ml alcopop bottle, a single measure of spirits or 100mls of wine.
Be more active and try to achieve a healthy weight
- Do whatever exercise you enjoy for example swimming, walking, cycling and gardening.
- The advice is at least 30 minutes of moderate intensity activity at least 5 days a week
- If you want to reduce your weight, or gain weight, ask to be referred to a dietitian who can help devise an individual plan for you.
Make time to relax
- Try reading, listening to music, relaxation or meditation tapes or taking up yoga or whatever you find relaxing.
Symptom specific advice
Constipation
- Drink 1.5-3L of fluid every day – water, decaffeinated drinks and herbal and fruit teas are good sources.
- Increase your fibre intake gradually from a variety of sources including oats, fruit, vegetables, linseeds and wholegrains.
- Try adding linseeds (golden or brown) to your diet, starting with 1 tablespoon per day of either whole or ground linseeds and building up to a maximum of 2 tablespoons (approx 24g) per day.
- Linseeds can be added to cereal, yogurt, soup or salad and should be accompanied by a drink (150ml fluid for every tablespoon of linseeds). Make this a daily routine as it may take up to 6 months to get the full benefit and the benefit will stop once you stop taking them.
- Those with diverticular disease tend to avoid whole seeds so you may choose to take milled linseed (called flaxseed) instead
- Avoid eating extra wheat bran
Wind and bloating
- Try to reduce/ limit gas producing foods e.g. onions, brussels sprout, cauliflower, beans and pulses.
- It may be helpful to eat oats (such as oat based breakfast cereal or porridge) and linseeds (up to 1 tablespoon per day).
Loose stool/Diarrhoea
- If you eat a lot of high-fibre foods consider reducing your intake of wholemeal and wholegrain breads and bran based breakfast cereals to see if it helps with symptoms. Try an oat based cereal instead.
- Avoid sorbitol, mannitol and xylitol. These are artificial sweeteners found in sugar-free sweets (including chewing gum) and drinks, and in some diabetic and slimming products.
- Replace lost fluids by drinking at least 6- 8 cups of fluid.
- Eating 3 portions of fresh fruit, spread throughout the day is fine, but avoid large volumes of fruit juice/ smoothies.
What if your symptoms do not improve after following the above advice?
Ask your doctor to refer you to a dietitian. A dietitian is clinically trained to assess your current diet and symptoms and tailor advice to meet your needs in a nutritionally balanced way.
If your IBS symptoms still persist despite the advice in this leaflet, the next recommended step includes a dietitian-led delivery of a low FODMAP diet.
The Low FODMAP diet is low in short- chain fermentable carbohydrates and recent research has shown that it can improve IBS symptoms in up to 75% of people with IBS. This diet is complex and must only be directed by a dietitian who has been trained in this area. Dietitians are the only nutrition professionals that have been trained to advise on the Low FODAMAP diet. Avoid getting information from the internet as the information may not be accurate or up-to-date and you could be at risk of nutritional deficiencies.
There is a lack of evidence to recommend a gluten-free diet or any specific food hypersensitivity intervention for treating IBS. if you feel that milk is causing you problems ask your GP for a lactose intolerance test or ask to be referred to a dietitian.
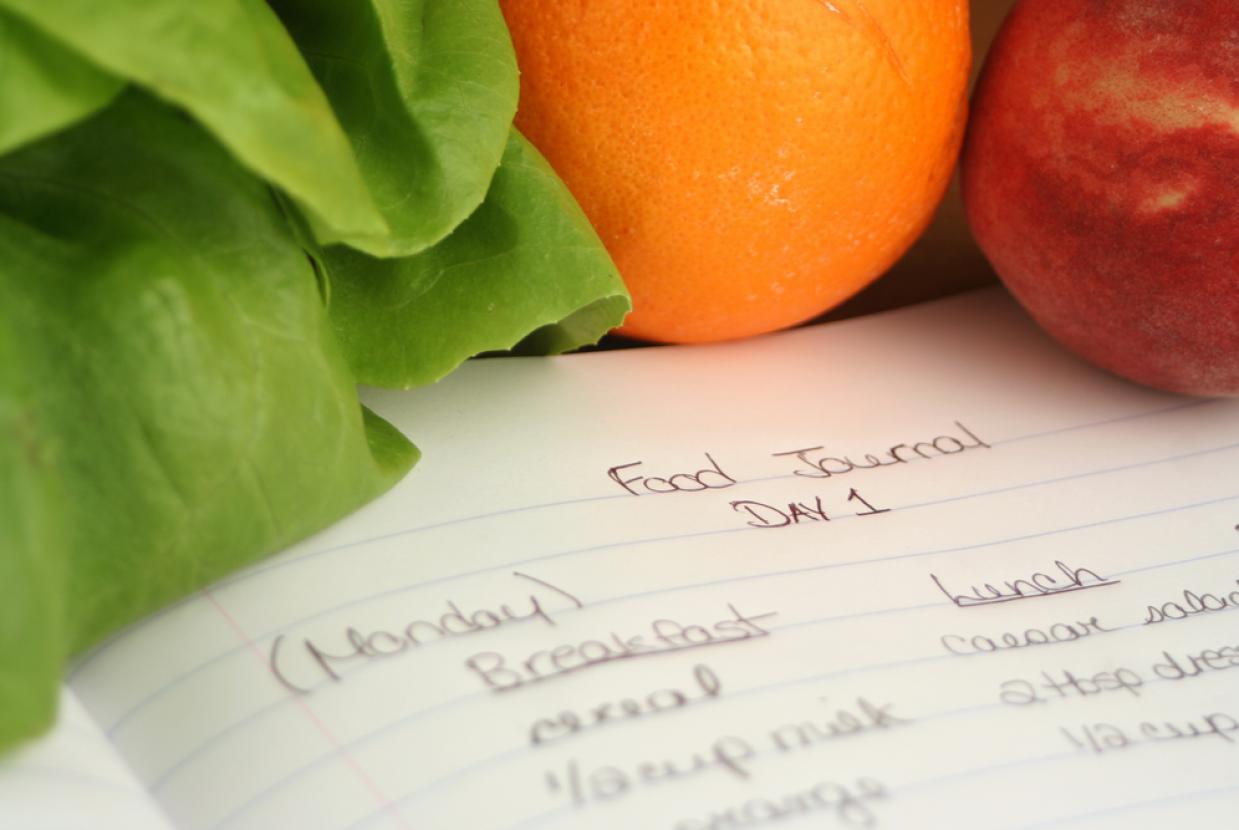
Should I keep a food and symptom diary?
Keeping a food and symptom diary can help you identify how certain foods and drinks affect your symptoms. Your dietitian can also use this to help identify patterns with your diet, lifestyle and symptoms.
Will food intolerance tests help to identify which foods I need to avoid?
Food intolerance tests are expensive and are not recommended as there is no convincing scientific evidence for their use. The test results can lead you to follow a diet that lacks many of the nutrients that you need. If you think you have intolerance to certain foods such as wheat or dairy foods, ask your doctor to refer you to a dietitian.
Probiotics
It is thought that these ‘friendly’ or ‘good’ bacteria may help IBS symptoms. However, good quality scientific research to recommend a specific probiotic for the treatment of IBS is lacking. You can choose probiotics in yoghurts, fermented milk drinks or tablet form. If you choose to try one of these products, include it daily for 1 month at the dose advised by the manufacturer. If you see no improvements, then you may consider an alternative brand.