HRT & The Menopause
Hormone replacement therapy (HRT) is a treatment used to help menopause symptoms. It replaces the hormones oestrogen and progesterone, which fall to low levels as you approach the menopause.
Menopause symptoms HRT can help to treat include:
- hot flushes
- night sweats
- sleep problems
- mood swings
- anxiety and low mood
- vaginal dryness
Menopause is when your periods stop due to lower hormone levels. It usually affects women between the ages of 45 and 55 but it can happen earlier. It affects anyone who has periods.
Oestrogen and progesterone are an essential part of period cycles, ovulation and pregnancy. They also keep your bones healthy. As you get older, the loss of these hormones can have a big effect on your body.
To replace these hormones, you'll usually take a combination of oestrogen and progestogen. If you've had a hysterectomy to remove your womb you can take oestrogen on its own.
Who can take HRT
You can usually take HRT if you're having menopause symptoms.
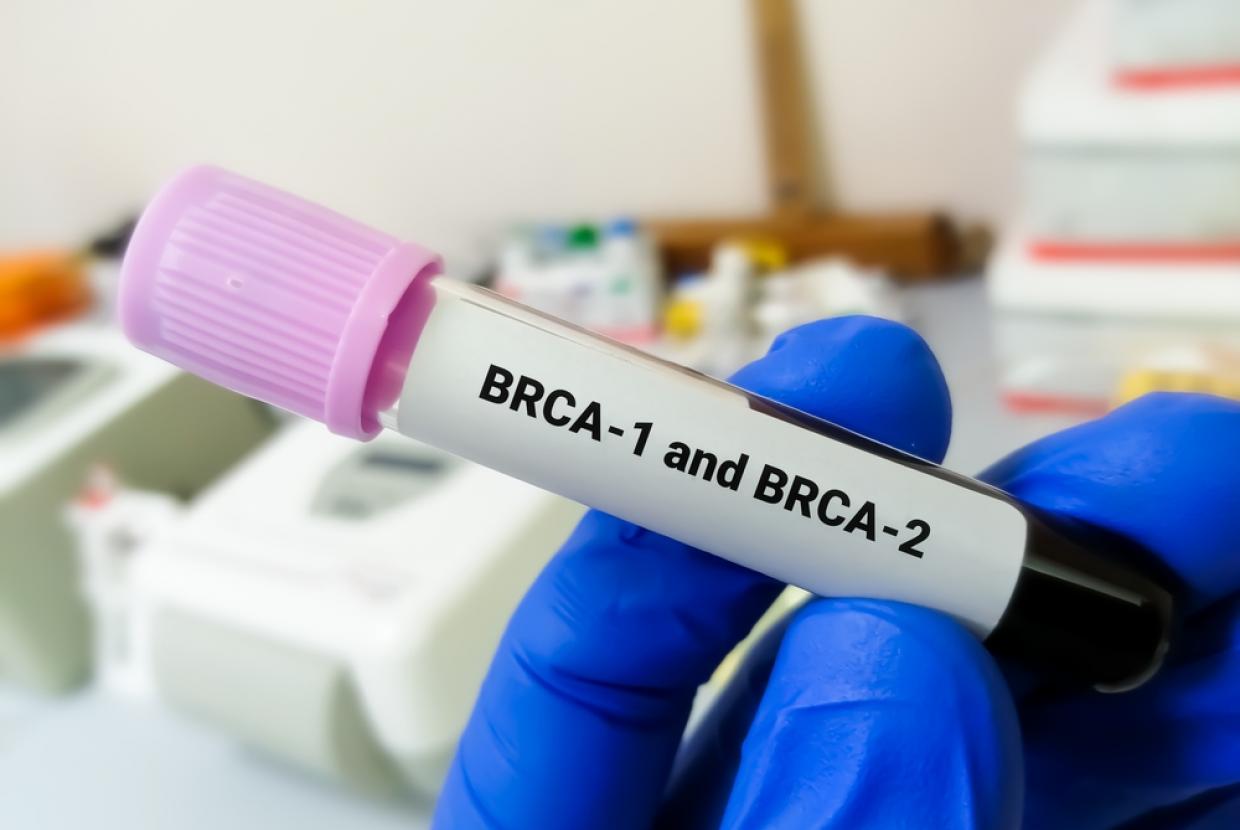
But HRT may not be suitable if you:
- have a history of breast cancer, ovarian cancer or womb cancer
- have a history of blood clots – you may need to use patches or gels rather than tablets
- have untreated high blood pressure – your blood pressure will need to be controlled before you can start HRT
- have liver disease
- are pregnant – it's still possible to get pregnant while taking HRT, so it's important to use contraception until 2 years after your last period if you're under 50, or for 1 year after the age of 50
If any of these apply to you, alternatives to HRT may be recommended instead.
Questions to ask your doctor
Before you see a GP, it's a good idea to be prepared so you get exactly what you need from the appointment.
If your periods have changed in recent months, make a note of it so you can tell the GP. Also tell them about any medicines or herbal remedies you're taking.
Your questions could include:
- how will HRT help me?
- how soon will I feel better?
- what are the benefits and what are the risks?
- is HRT the only treatment I can have for my symptoms?
- how long will I have to take it for?
- how will I know what type will work best for me?
A GP should be able to answer your questions and help you choose the type of HRT that's suitable for you.
After you start taking HRT
You'll usually start with a low dose, which may be increased later. Your symptoms should improve after a few days or weeks.
A GP will usually recommend a review appointment 3 months after you start taking HRT, or if you change your type of HRT. This is to see how well it's working. If everything is OK, you'll usually have 1 review a year.
If your symptoms do not improve or you get side effects, a GP may suggest either:
- changing your dose
- changing the type of HRT you're taking
- referring you to a menopause specialist doctor.
You'll usually need to take HRT for 2 to 5 years, but it can be longer in some cases.
If you do decide to take or use HRT, find out how to save money on your medicines with a prescription prepayment certificate.
Further information
Types of HRT
There are many types of HRT, including different hormones and different ways to take or use it, such as tablets, patches or gel. Finding the right one for you can take some time.
A GP can help you choose what type, method and treatment cycle is best for you.
Benefits and risks
The main benefit of HRT is that it can help with most menopause symptoms, such as hot flushes, mood swings and vaginal dryness. It can also help prevent weakening of the bones (osteoporosis).
Side effects of HRT
Like any medicine, HRT can cause side effects, but not everyone gets them. If you do get side effects, they're usually mild and pass within 3 months of starting treatment.
When to take HRT
It may be difficult to know when to start HRT, how long to take it for and when to stop it. You may also want to know if you can take it while using contraception.
Alternatives to HRT
If you're unable to take HRT or decide not to, you may want to consider other ways of controlling your menopause symptoms. These may include lifestyle changes, other medicines or herbal remedies.