Treating Endometriosis
Treatments for endometriosis
It’s not known what causes endometriosis and there are currently no treatments that can cure it. But treatment can help manage symptoms such as pain.
Your doctor will talk to you about the risks and possible side effects of each treatment.
If treatment is not working or your symptoms are very severe, you may be referred to a specialist endometriosis service.
Medicines for endometriosis
Medicines are often the first treatment for endometriosis. They include:
- painkillers, such as paracetamol and ibuprofen
- hormones, such as the combined contraceptive pill – these can help ease pain
You will not be given hormones if you're trying to get pregnant.
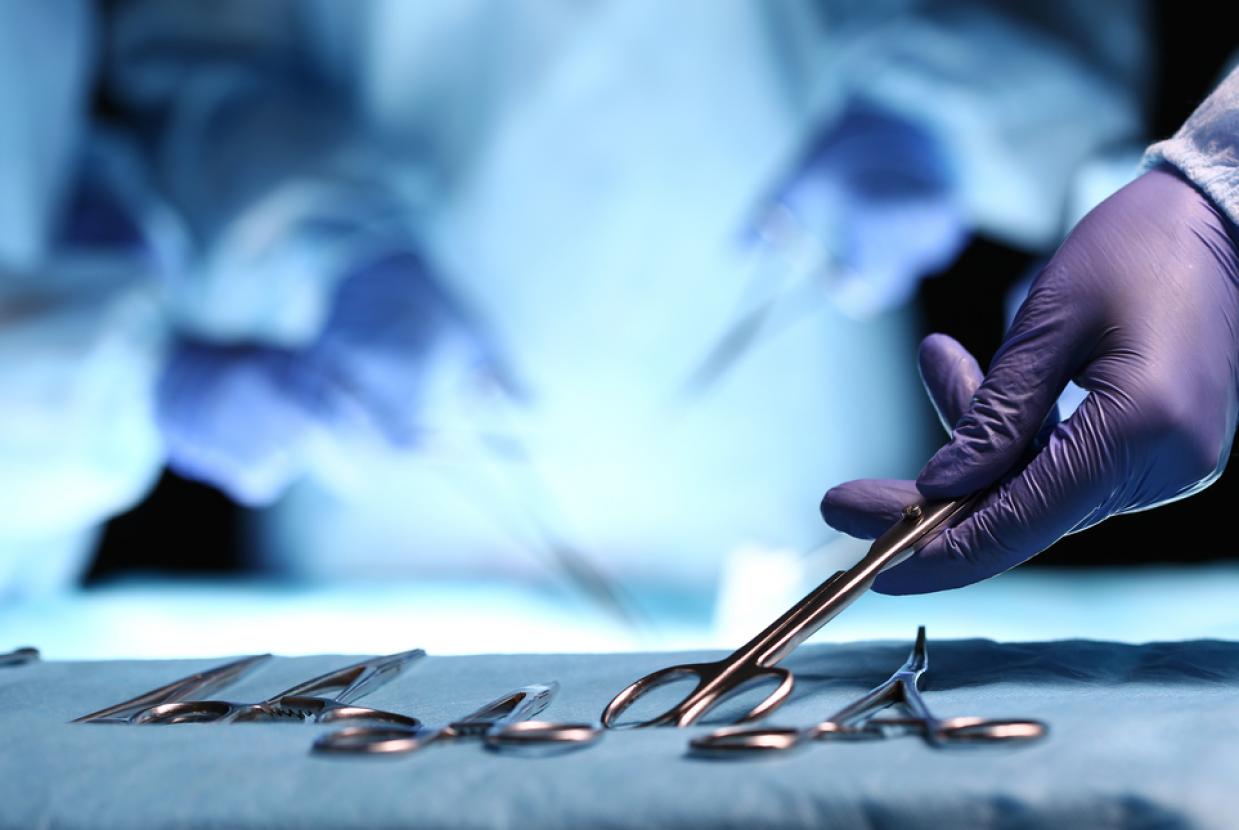
Surgery for endometriosis
If other treatments are not working or you have lots of endometriosis, you may be offered surgery. Surgery is also an option if endometriosis is affecting your ability to have children.
You can have surgery to:
- remove areas of endometriosis or fluid-filled sacs (ovarian cysts) caused by endometriosis
- remove your womb (hysterectomy) or ovaries (oophorectomy)
- remove part of your bladder or bowel, if endometriosis is affecting these
You may need to have more surgeries if your symptoms come back after your first surgery, or if surgery causes scarring that makes your organs to stick together (adhesions).