Foot & Ankle Pain
Most people experience pain in and around their feet or ankles at some point in their lives. It’s one of the most complex, hard-working regions of your body. It has 26 bones and 33 small joints, all held together by a network of soft tissue made up of muscles, tendons, ligaments, nerves, and blood vessels.
Most cases of foot or ankle pain are short term and are caused by soft tissue injuries, such as sprains or strains. These should gradually heal with the help of simple self-care measures. Though some could take a few months to fully recover, you probably won’t need to seek treatment from a healthcare professional.
However, some pain can have no obvious cause or may not improve significantly with self-care. Pain that seems to be getting worse, does not improve, or lasts longer than a few months could be due to structural changes in the foot or ankle, or an underlying condition.
There can be several explanations for long-term pain in and around the feet or ankles, such as:
- badly fitting footwear
- osteoarthritis
- inflammatory arthritis
- connective tissue diseases
- poor blood circulation
- nerve damage.
When should I see a healthcare professional about foot or ankle pain?
Some foot pain can become more than a short-term problem. If you cannot treat the pain yourself or you have a condition that could affect the joints or soft tissue, it may need further investigation.
You should speak to your doctor or a footcare specialist if:
- your pain does not improve in the first few days
- your pain is getting worse
- it is still causing problems after two weeks of self-care
- you have sores that are not healing
- your skin has changed colour – especially if it’s turned dark blue or black
- your foot has changed shape or is really swollen
- you have a high temperature or feel hot and shivery
- it is red, warm, or swollen – as you may have an infection
- the problem keeps coming back or lasts longer than three months
- you have an inflammatory condition, such as rheumatoid arthritis or scleroderma
- you have diabetes
- you are taking steroids, biologics or other drugs that affect your immune system.
Your doctor may want to refer you to a specialist in foot care, such as a podiatrist, physiotherapist, or an orthotist, for a diagnosis and treatment.
How can I treat foot or ankle pain when it starts?
Most foot or ankle pain can be treated without the need to see a healthcare professional. Soft-tissue injuries should begin to improve over the first few days with the help of some simple self-care tips. You may need to be careful and protect the injured area for several months, until it has fully recovered.
Self-care tips
Paracetamol and pain-relieving gel should help reduce your pain and discomfort. There are four steps to treating pain, known as RICE therapy, which can help improve healing, particularly in the first 2-3 days, these are:
- Rest – try to avoid putting weight on the injured foot or ankle. Do not exercise, instead try gently moving it from time to time to stop the area getting stiff.
- Ice – put an ice pack or frozen vegetables, covered in a damp cloth, on the painful area for 20 minutes every 2-3 hours.
- Compression – wrap a bandage around the area that’s painful. It should be tight enough to support it, but not so tight that it restricts the blood flow. If you’ve hurt your toe place a small piece of cotton wool between it and the next toe, then tape them together.
- Elevate your foot to reduce swelling.
By gently massaging the painful area from time to time you can help reduce swelling and increase blood flow. It is best to avoid hot baths, heat packs, ibuprofen, and alcohol in the first few days, as they can affect healing.
Exercise
Exercise can help reduce pain and stiffness in the feet and ankles. You can find examples of exercises that could help you on our exercises for the toes, feet and ankles page.
If your feet or ankles are stiff in the morning you may find it easier to exercise once they have had time to loosen up. A warm bath or shower can help ease stiffness.
Start gently and slowly build up the amount you are doing once each exercise becomes easier or more comfortable.
It’s normal to feel some slight aches as you move your foot or ankle. However, if movement makes it feel worse or is causing bursts of more intense pain, stop and consult a healthcare professional.
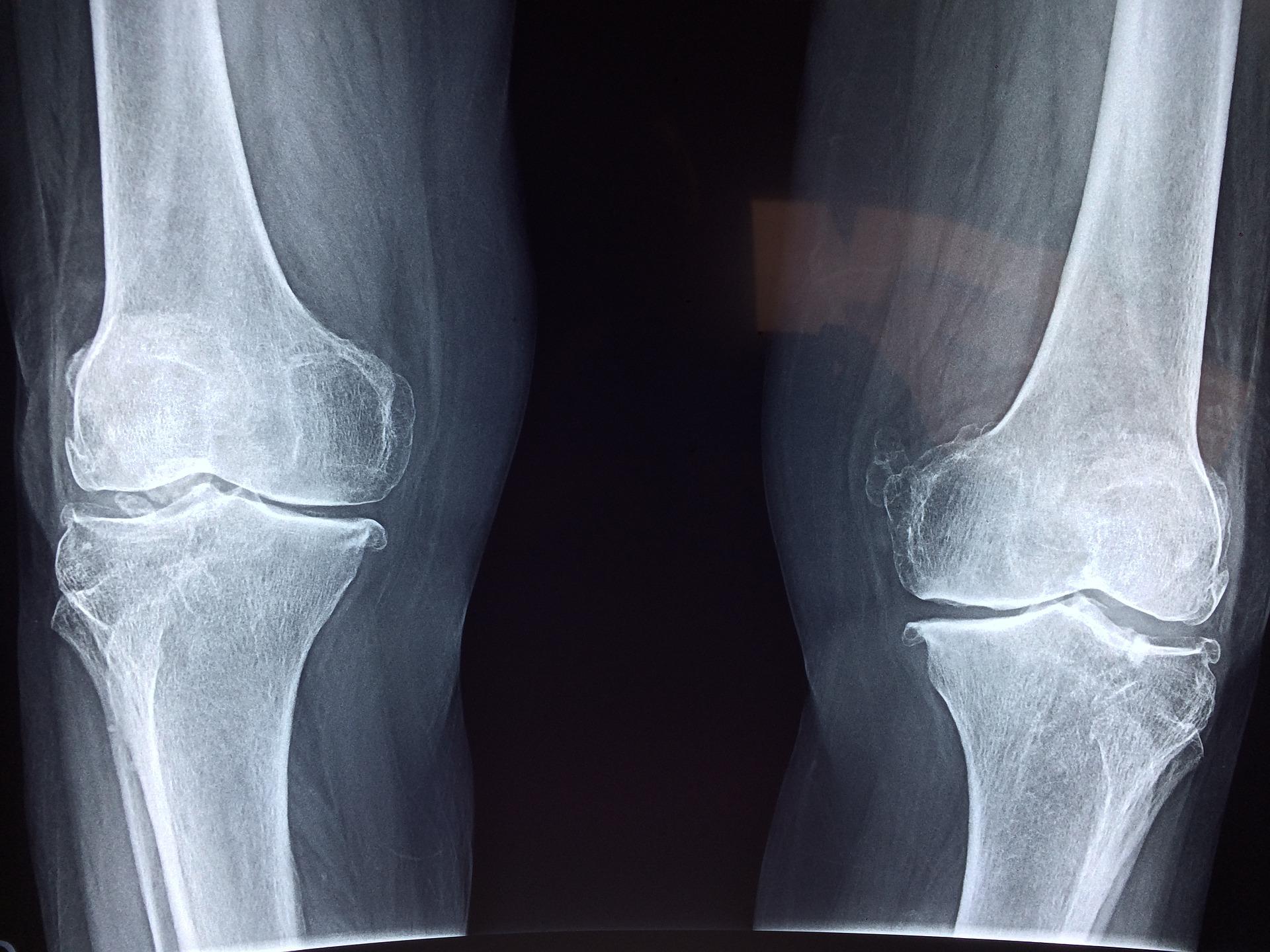
How can arthritis affect your feet?
Several types of arthritis can affect your feet and ankles. Some, such as osteoarthritis, can be managed with painkillers, non-steroidal anti-inflammatory drugs (NSAIDs) and exercises that strengthen and stretch the soft tissue around the affected joint.
If your pain doesn't improve, your doctor may recommend a steroid injection into the joint to reduce the swelling and pain and get your foot and ankle moving more.
However, inflammatory conditions such as rheumatoid arthritis are likely to need disease-modifying anti-rheumatic drugs (DMARDs) or biologics. These long-term treatments should address the inflammation causing your pain.
Gout
Gout is a very painful type of arthritis. It is caused by crystals collecting inside a joint and commonly affects the foot, particularly the big toe.
During a gout attack the joint can be inflamed for up to two weeks. Without medication, further attacks can cause permanent damage to the joint, which could then lead to osteoarthritis.