Heart Disease, Stroke & Diet
What is heart disease and stroke?
Heart disease and stroke are major causes of death worldwide. In the UK, one in eight men and one in fourteen women die from heart disease.
The number of deaths from heart disease have been decreasing in recent years but it is still one of the major causes of premature death (before 75 years) in the UK and a leading cause of ill health.
But the good news is - both heart disease and stroke are largely preventable!
Eating a healthy diet can help reduce your risk of heart disease and stroke.
What causes heart attacks and strokes?
The condition that causes most heart attacks and strokes is known as atherosclerosis.
- Atherosclerosis is the build-up of fatty material inside arteries (blood vessels) like the coronary arteries that supply blood to the heart.
- The build-up of fatty material causes a narrowing in the artery, and as these become more severe, they can restrict the flow of blood so not enough blood can reach the heart.
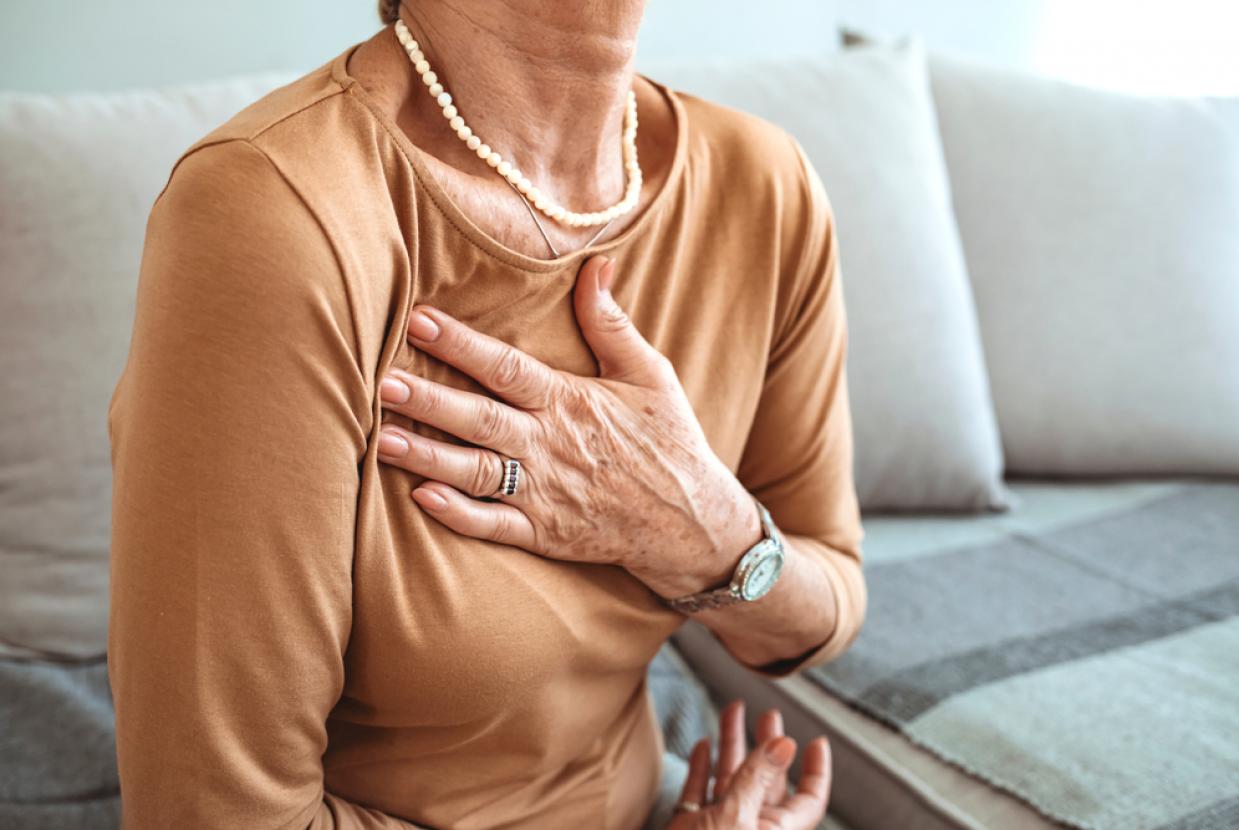
- This can cause the symptoms of angina (such as chest pain and shortness of breath).
- If the fatty material breaks down (or ruptures), a blood clot can form, which can completely block the artery and lead to a heart attack.
- Strokes occur if blockages or ruptures occur in blood vessels in the brain.
It's important to make healthy diet and lifestyle choices when it comes to heart health.
Key Facts about heart disease and stroke
- Giving up smoking is one of the best things you can do to protect your heart.
- We need to keep active and should aim for at least 150 minutes a week of moderate physical activity.
- We should not drink to excess – adults should drink no more than 14 units a week, with several alcohol-free days each week.
- We should aim for a healthy body weight.
Who is at risk of heart disease and stroke?
There are several risk factors for atherosclerosis and heart disease. A risk factor is something that increases your chance of getting a disease.
The more risk factors you have, the greater your personal risk. But there are many things you can do to reduce your overall risk and keep your heart healthy.
Risk factors for heart disease and stroke
High blood pressure (hypertension) - Having high blood pressure puts strain on your heart that can lead to your blood vessels becoming damaged, making them more at risk of heart disease.
Smoking - Quitting smoking is the single best thing you can do for your heart health.
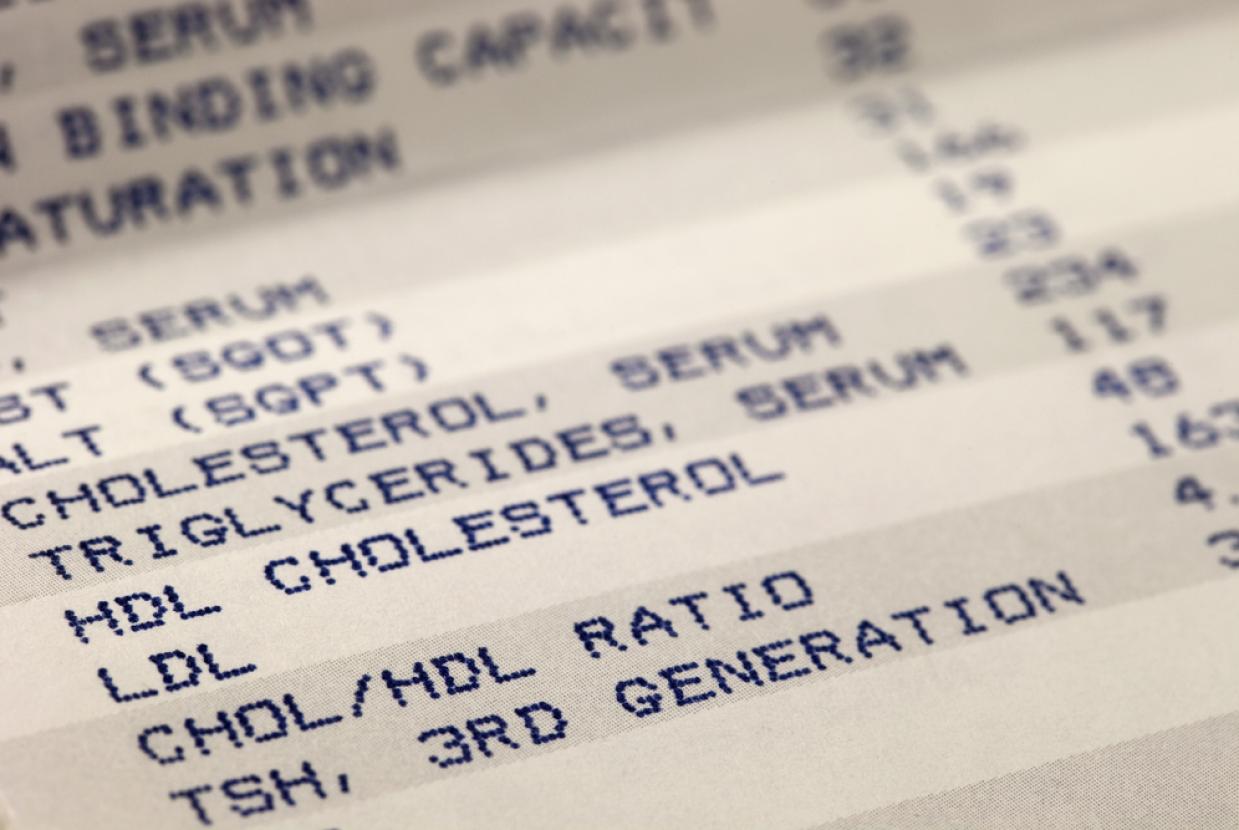
High blood cholesterol - High levels of cholesterol (a type of fatty substance) in the blood can build up in the walls of the coronary arteries, restricting blood flow to the heart and rest of the body.
Diabetes - The increased levels of blood glucose that can occur in type 1 and type 2 diabetes can damage the coronary arteries, increasing the chances of heart disease developing.
Lack of exercise - Not exercising regularly increases the chance of high blood pressure, higher cholesterol levels and overweight and obesity. These are all risk factors for developing heart disease.
Being overweight or obese - Research shows that being overweight or obese can raise your blood cholesterol levels, increase your blood pressure and increase your risk of developing type 2 diabetes.
Family history of heart disease - You are considered to have a family history of cardiovascular disease (CVD) if your father or brother was under age 55 years when they were diagnosed with CVD, or your mother or sister was under age 65 years when they were diagnosed with CVD.
Ethnic background - For the South Asian population (Bangladeshis, Indians and Pakistanis), and people with an African Caribbean background, CVD risk can be higher than for the rest of the UK population.
Age - Your risk of developing heart disease increases with age.
Gender - Men are more likely to develop heart disease earlier than women.
How do I reduce my risk of heart disease and stroke?
Even though you cannot do anything to change some of these risk factors, there are several lifestyle behaviours which put you at increased risk that can be changed.
Smoking
You are nearly twice as likely to have a heart attack if you smoke compared to people who have never smoked. Therefore, giving up smoking is one of the most important things you can do to protect your heart. If you’re thinking about quitting smoking, find out more about what help and support is available from your local Stop Smoking Service on this NHS webpage.
Drinking too much alcohol
Regularly drinking more alcohol than we are recommended over a long period of time raises blood pressure, which is a risk factor for heart disease and stroke. It can also weaken the heart muscle so the heart cannot work as well. Binge drinking (drinking more than six units a day for women or eight units a day for men) is a risk factor for heart disease. The recommendations for alcohol to keep any health risks low are that: men should not drink more than 14 units of alcohol each week, the same level as for women. Men and women should have several alcohol-free days each week.
Lack of physical activity
Being inactive is a major health risk and one of the main causes of death and ill health in the UK. You should aim for 150 minutes of moderate intensity physical activity (when you feel warm and slightly out of breath) a week. Talk to your GP before starting on a new exercise programme, especially if you have a history of heart disease, stroke or other health problems.
A poor diet
Healthy diets that include wholegrains, fruit and vegetables, nuts and seeds, oily fish and choosing unsaturated fats (such as the Mediterranean diet) are important for good heart health.
These factors contribute to the risk of obesity, type 2 diabetes, high blood pressure and high cholesterol levels, which are some of the strongest risk factors for heart disease.
For further information visit - Nutritional information about heart disease and stroke