Folic Acid
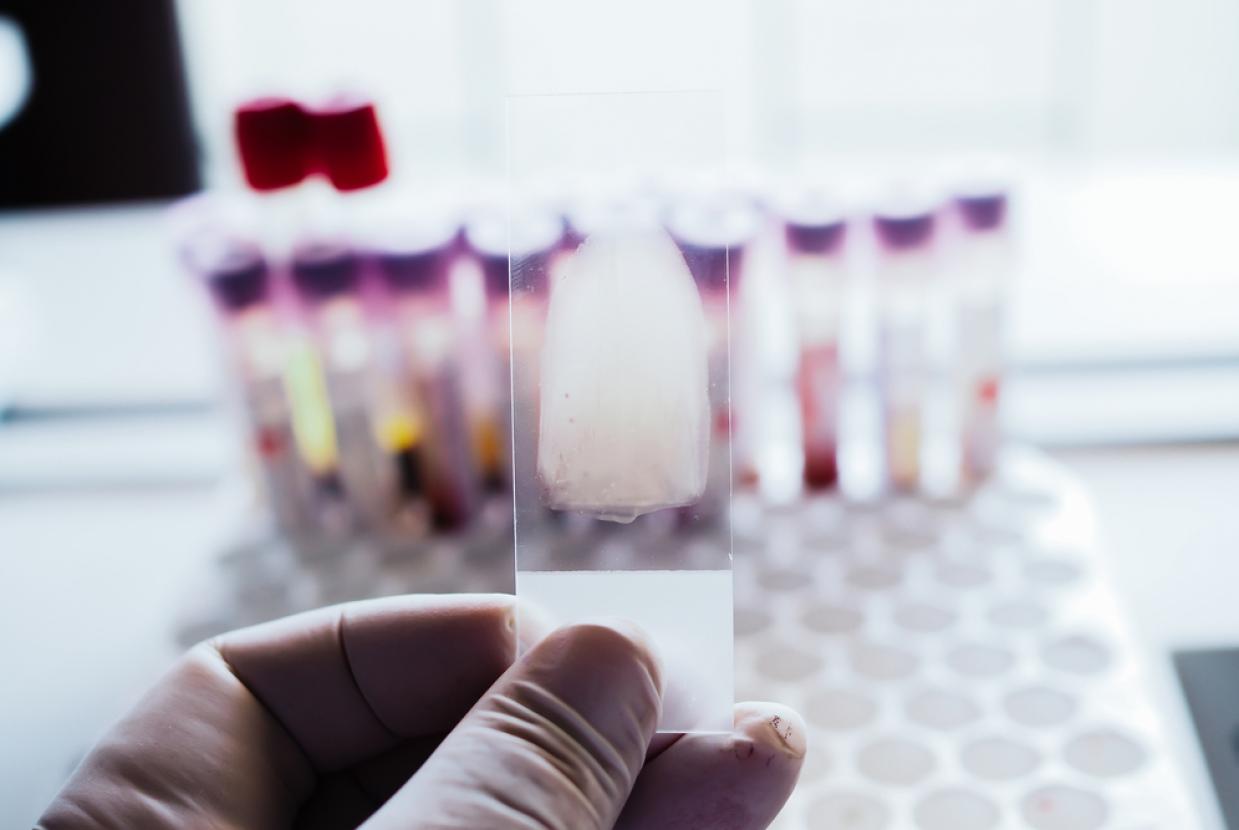
Folic acid is a B vitamin which is vital for the formation of red blood cells. It supports growth and cell division in the body. The form of folic acid occurring naturally in food is called ‘folate’.
What is folic acid and who needs it?
Folic acid, together with vitamin B12, is necessary to form red blood cells. A deficiency of folic acid can reduce the ability of red blood cells to carry oxygen. This is called ‘macrocytic’ (large cell) anaemia. Together, both vitamins also help nerves to function properly.
Folic acid is also essential in the formation of DNA (genetic material) within every body cell, allowing each cell to replicate. Everyone needs sufficient folate or folic acid in their diet to maintain health, but more is needed in the preconception period and during pregnancy and breastfeeding because requirements are increased.
How much folic acid do I need?
If you are not likely to become pregnant, you should be able to obtain enough folate by eating a healthy diet containing a wide variety of foods.
Pregnancy and lactation (breastfeeding)
A foetus rapidly develops spine and nerve cells in the first few weeks of pregnancy. Inadequate levels of folate at this crucial time increase the risk of the baby’s spine developing a ‘neural tube defect’, resulting in spinal malformation called spina bifida. For this reason, anyone considering pregnancy, and up to 12 weeks of pregnancy is advised to:
- Take a folic acid supplement, or pregnancy specific vitamin supplement providing 400μg every day
- Eat a diet rich in folate and folic acid from foods naturally containing the vitamin and from fortified foods
During the whole of pregnancy and lactation, it is advisable to eat a diet rich in folate as requirements for the vitamin are higher.
Daily recommendations for folate (folic acid) intake
(μg = micrograms, mg = milligrams)
- Adults and children over 11 years: 200μg
- Anyone considering pregnancy: 200μg plus a supplement* containing 400μg
- If you are pregnant: 300μg plus a 400μg supplement* during the first 12 weeks of pregnancy
- If you are breastfeeding: 260μg
(*You may need to take 5mg/day of folic acid preconception and up to 12 weeks of pregnancy, if you have had a pregnancy previously affected by neural tube defects, if you have diabetes, if you are living with obesity, or take anti-epilepsy medication. Ask your doctor as this will need to be provided on prescription.)
Which foods contain folic acid?
Folate is found naturally in a wide variety of foods and is also present in foods fortified with folic acid. As it is a water-soluble vitamin (dissolves easily in water), it is lost from food during cooking. This can be reduced by steaming or microwaving vegetables instead of boiling and avoiding over-cooking.
Good sources of folate / folic acid are:
- Spinach, kale, Brussels sprouts, cabbage, broccoli
- Beans and legumes (e.g. chickpeas, lentils, blackeye beans, kidney beans)
- Fortified foods (e.g. some brands of breakfast cereals – check the label)
- Nuts and seeds
- Yeast and beef extracts
- Oranges and orange juice
- Wheat bran and other wholegrain foods
- Eggs
- Poultry, pork, shellfish and liver
Which foods are fortified with folic acid?
Despite recommendations, many women do not take folic acid supplements in early pregnancy and many pregnancies are unplanned. Routine fortification of flour with folic acid is a simple way to increase folic acid intake for everyone. Many countries, such as the USA and Canada, have introduced mandatory fortification of flour with folic acid, and have seen a significant reduction of the number of births affected by neural tube defects. The UK government is committed to introducing the mandatory addition of folic acid to non-wholemeal wheat flour and has recently consulted on how this will be carried out.
What happens if I don’t get enough folic acid?
Folic acid deficiency can result in tiredness, weakness, diarrhoea, loss of appetite and weight loss. A lack of folic acid can also cause headaches, heart palpitations, a sore tongue and behavioural disorders.
Sometimes you can become deficient because you are losing lots of folic acid (if you suffer from Crohn’s disease or untreated coeliac disease (for example), if you are using certain medications such as water tablets (diuretics), or if you are consuming too much alcohol.
Can I take too much folic acid?
It is advisable for the over-50s or those with a history of bowel cancer, not to take folic acid supplements containing more than 200μg/day. You should also not take folic acid supplements if you have vitamin B12 deficiency - unless advised to do so by your doctor. If you have been prescribed folic acid because you have a high risk of neural tube defects, or because you have folate deficiency, or to help with another medical condition, follow the advice of your doctor. For other people, long-term intakes of folic acid from fortified foods and supplements should be below 1mg/ day for adults (lower amounts for children).
Top tips
- Eat a wide variety of green vegetables (such as spinach, cabbage, kale, broccoli)
- Steam vegetables or boil with a small amount of water for a short time
- Use cooking water from vegetables for gravy, sauces, or soup
- Include wholegrain cereals, beans and peas in your diet
- When choosing a breakfast cereal, check the label to ensure it is fortified with folic acid
- If planning a pregnancy take a 400ug folic acid supplement (continue to take it until week 12 of pregnancy)
- If you are planning a pregnancy and you are at higher risk of neural tube defects - ask your doctor about taking a 5mg folic acid supplement