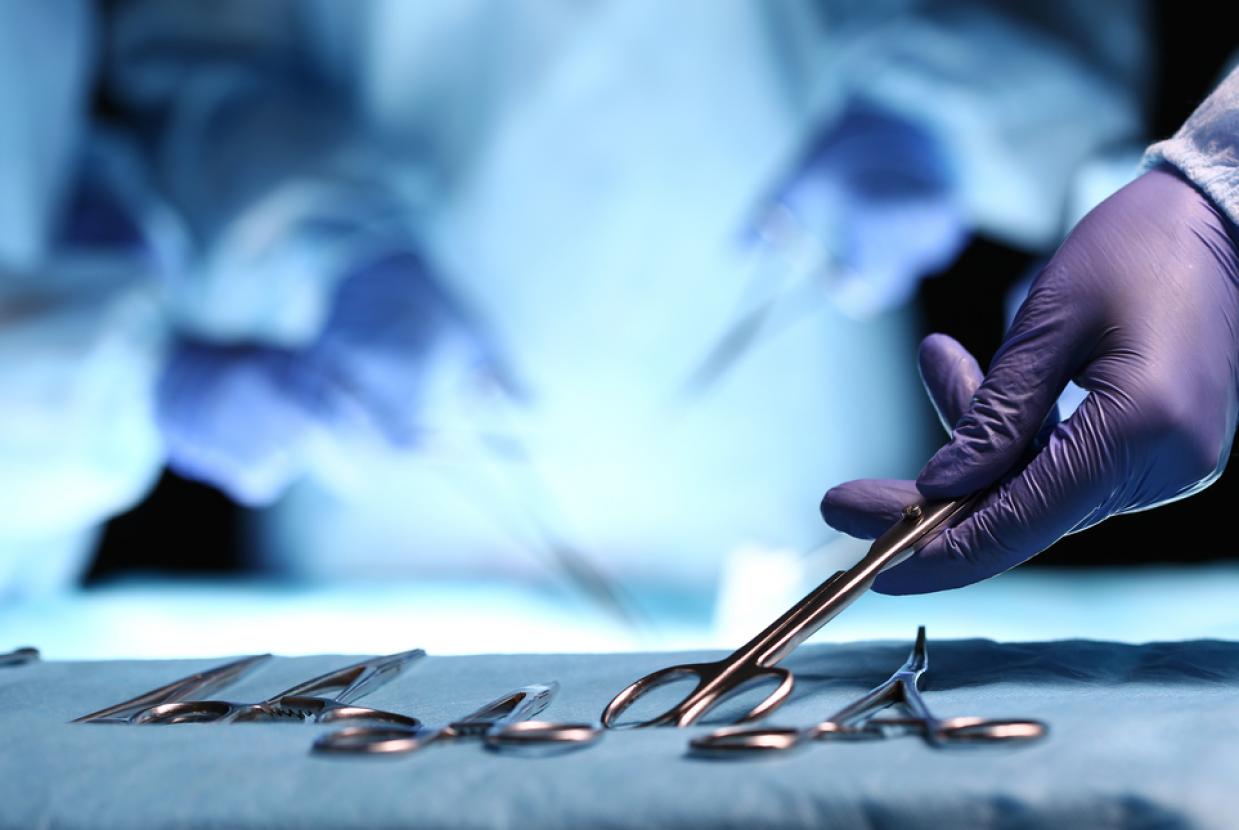
Surgery & Procedures
If non-surgical treatments for urinary incontinence are unsuccessful or unsuitable, surgery or other procedures may be recommended. Before making a decision, discuss the risks and benefits with a specialist, as well as any possible alternative treatments.
Your doctor must keep a detailed record of the type of surgery they do, including any complications you get after you have had surgery. You should be given a copy of this record.
If you plan to have a pregnancy, this will affect your options. The physical strain of pregnancy and childbirth can sometimes cause surgical treatments to fail. You may wish to wait until after you have had children before you choose surgery.
Surgery and procedures for stress incontinence
Colposuspension
Colposuspension involves making a cut in your lower tummy (abdomen), lifting the neck of your bladder, and stitching it in this lifted position. If you have a vagina, a colposuspension can help prevent involuntary leaks from stress incontinence.
There are 2 types of colposuspension:
- open colposuspension – where surgery is done through a large cut
- laparoscopic (keyhole) colposuspension – where surgery is done through 1 or more small cuts using small surgical instruments
Both types of colposuspension offer effective long-term treatment for stress incontinence, although laparoscopic colposuspension needs to be done by an experienced laparoscopic surgeon. Problems that can happen after colposuspension include difficulty emptying the bladder completely when peeing, urinary tract infections (UTIs) that keep coming back, and discomfort during sex.
Sling surgery
Sling surgery involves making a cut in your lower tummy (abdomen) and vagina so a sling can be placed around the neck of the bladder to support it and prevent urine leaking.
The sling can be made of:
- tissue taken from another part of your body (autologous sling)
- tissue donated from another person (allograft sling)
- tissue taken from an animal (xenograft sling), such as cow or pig tissue
In many cases, an autologous sling is used. It is made from part of the layer of tissue that covers the abdominal muscles (rectus fascia). These slings are generally preferred because more is known about their long-term safety and effectiveness. Sling surgery can cause side effects, including continued or new problems urinating. Speak to your doctor about the risk of side effects.
Vaginal mesh surgery (tape surgery)
At the moment, it may not be possible to have vaginal mesh surgery for urinary incontinence on the NHS. But you should have a detailed discussion with a specialist to talk about your options.
Vaginal mesh surgery is where a strip of synthetic mesh is inserted behind the tube that carries urine out of your body (urethra) to support it. Vaginal mesh surgery for stress incontinence is sometimes called tape surgery. The mesh stays in the body permanently.
You'll be asleep during the operation. It's often done as day surgery, so you do not need to stay in hospital. Some people need to stay in hospital overnight. A few people have had serious complications after mesh surgery. Some, but not all, of these complications can also happen after other types of surgery.
Problems include:
- long-lasting pain
- permanent nerve damage
- incontinence
- constipation
- sexual problems
- mesh exposure through vaginal tissues and occasionally injury to nearby organs, such as the bladder or bowel
If you have previously had vaginal mesh or tape inserted for incontinence and you think you're having complications, speak to a GP or your surgeon. If you're not having any complications, there's no need to do anything. Many women have had these types of surgery without developing any problems afterwards.
Urethral bulking agents
A urethral bulking agent is a substance that's injected into the walls of the urethra in people with stress incontinence who have a vagina.
This increases the size of the urethral walls and allows the urethra to stay closed with more force. Several different bulking agents are available, and there's no evidence 1 is more beneficial than another.
This is less invasive than surgical treatments for stress incontinence in people with a vagina, as it does not usually require any cuts. The substance is usually injected through a cystoscope (a thin camera) inserted into the urethra.
Urethral bulking agents are generally less effective than other procedures. The effectiveness of a urethral bulking agent will also reduce with time and you may need the injection to be repeated. Many people experience a slight burning sensation or bleeding when they pass urine for a short period after a bulking agent is injected.
Artificial urinary sphincter
The urinary sphincter is a ring of muscle that prevents urine flowing from the bladder into your urethra.
In some cases, it may be suggested that you have an artificial urinary sphincter fitted to relieve your incontinence.
This treatment is used more often for people who have a penis rather than a vagina.
An artificial sphincter has 3 parts:
- a circular cuff that's placed around the urethra – this can be filled with fluid when necessary to compress the urethra and prevent urine passing through it
- a small pump placed in the scrotum (when used in people who have a penis) that contains a mechanism for controlling the flow of fluid to and from the cuff
- a small fluid-filled reservoir in the tummy – the fluid passes between this reservoir and the cuff as the device is activated and deactivated
The procedure to fit an artificial urinary sphincter often causes short-term bleeding and a burning sensation when you pee. It's not uncommon for the device to eventually stop working, in which case further surgery may be needed to remove it
Surgery and procedures for urge incontinence
Botulinum toxin A injections
Botulinum toxin A (Botox) can be injected into the sides of your bladder to treat urge incontinence and overactive bladder syndrome.
This medicine can sometimes help relieve these problems by relaxing your bladder. This effect can last for several months and the injections can be repeated if they help. Although the symptoms of incontinence may improve after the injections, you may find it difficult to completely empty your bladder.
If this happens, you'll need to be taught how to insert a thin, flexible tube called a catheter into your urethra to drain the urine from your bladder. The long-term effects of this treatment are not yet known.
Sacral nerve stimulation
The sacral nerves are located at the base of your back. They carry signals from your brain to some of the muscles used when you go to the toilet, such as the detrusor muscle that surrounds the bladder.
If urge incontinence is the result of your detrusor muscles contracting too often, sacral nerve stimulation, also known as sacral neuromodulation, may be recommended. A device is inserted near 1 of your sacral nerves, usually in 1 of your buttocks. An electrical current is sent from the device into the sacral nerve.
This should improve the way signals are sent between your brain and your detrusor muscles and reduce your urges to pee. Sacral nerve stimulation can be painful and uncomfortable, but some people report a substantial improvement in their symptoms or the end of their incontinence completely.
Posterior tibial nerve stimulationYour posterior tibial nerve runs down your leg to your ankle. It contains nerve fibres that start from the same place as nerves that run to your bladder and pelvic floor.
It's thought that stimulating the tibial nerve will affect these other nerves and help control the urge to pee.
A very thin needle is inserted through the skin of your ankle and a mild electric current is sent through it, causing a tingling feeling and your foot to move.
You may need 12 sessions of stimulation, each lasting around 30 minutes, 1 week apart.
Some studies have shown that this treatment can offer relief from urge incontinence and overactive bladder syndrome for some people, although there's not enough evidence yet to recommend tibial nerve stimulation as a routine treatment.
Tibial nerve stimulation is only recommended in a few cases where urge incontinence has not improved with medicine and you do not want to have botulinum toxin A injections or sacral nerve stimulation.
Augmentation cystoplasty
In rare cases, an operation known as augmentation cystoplasty may be recommended to treat urge incontinence. This involves making your bladder bigger by adding a piece of tissue from your intestine into the bladder wall. After augmented cystoplasty you may not be able to pass urine normally and may need to use a catheter.
Because of this, augmentation cystoplasty is only considered if you're willing to use a catheter. The difficulties passing urine can also mean that people who have augmentation cystoplasty can get urinary tract infections (UTIs) that keep coming back.
Urinary diversion
Urinary diversion is a procedure where the tubes that lead from your kidneys to your bladder (ureters) are redirected to the outside of your body.
The urine is then collected in a bag, without it flowing into your bladder. Urinary diversion should only be done if other treatments have been unsuccessful or are not suitable. It can cause several complications, such as a bladder infection, and sometimes further surgery is needed to correct any problems that happen.
Catheterisation for overflow incontinence
There are 2 types of catheterisation for overflow incontinence, clean intermittent catheterisation and indwelling catheterisation.
Clean intermittent catheterisation (CIC)
Clean intermittent catheterisation (CIC) is used to empty the bladder at regular intervals and so reduce overflow incontinence, also known as chronic urinary retention.
A continence adviser will teach you how to pass a catheter through your urethra and into your bladder. Urine will then flow through the catheter and into the toilet. Using a catheter can feel a bit painful or uncomfortable at first, but discomfort should ease over time.
How often CIC will need to be done will depend on your circumstances. For example, you may only need CIC once a day, or you may need to use it several times a day. Regular use of a catheter increases the risk of urinary tract infections (UTIs).
Indwelling catheterisation
If using a catheter occasionally is not enough to treat overflow incontinence, you can have an indwelling catheter fitted instead. This is a catheter that's inserted in the same way as CIC, but left in place. A bag is attached to the end of the catheter to collect urine.