World Ovarian Cancer Day
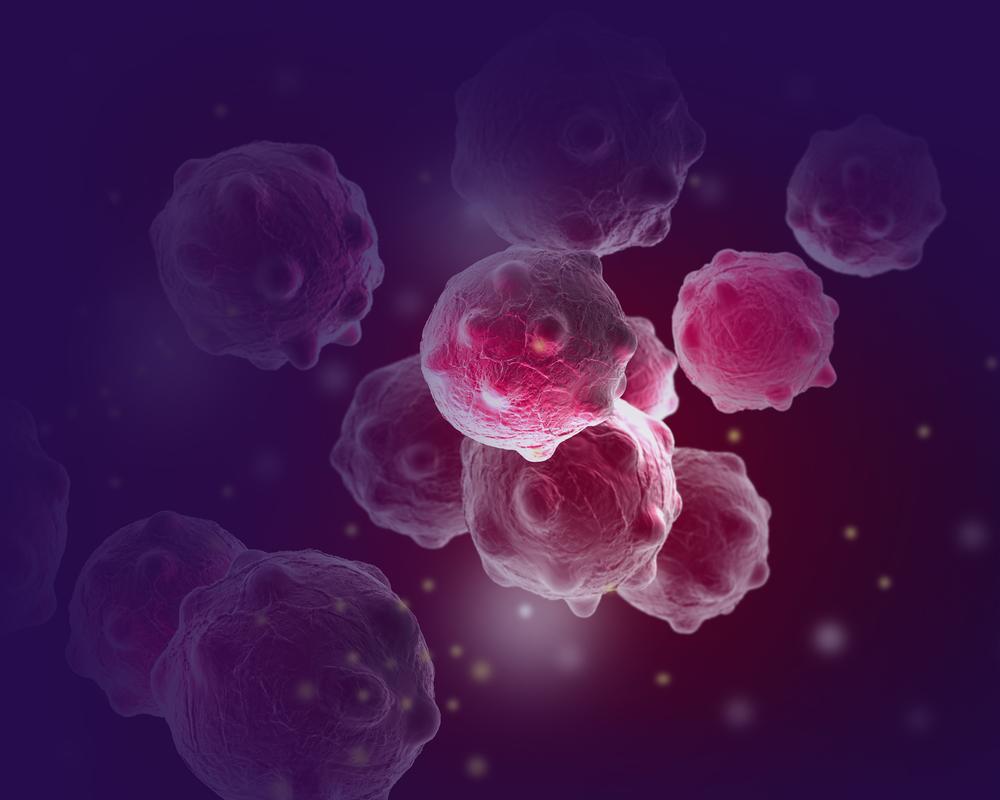
Cancer / Women's HealthThe ovaries are 2 small, oval-shaped organs in the pelvis (lower area between the hips). They are on either side of the womb (uterus), close to the fallopian tubes. These link the ovaries to the womb. A layer of tissue called the peritoneum supports the ovaries.
About 7,400 women are diagnosed with cancer of the ovary (ovarian cancer) each year in the UK. The surface of the ovaries, fallopian tubes and peritoneum are very close together. Doctors think most ovarian cancers start in the cells at the end of the fallopian tube and travel to the ovaries or the peritoneum.
Cancers of the ovary, fallopian tube and of the peritoneum are often grouped together because they are so similar. They are treated in the same way. Ovarian cancer can affect anyone who has ovaries and fallopian tubes. This includes women, transgender (trans) men and people assigned female at birth.
Symptoms of ovarian cancer
Cancer of the ovary causes symptoms like other more common and less serious conditions. This can make it more difficult to diagnose it early. Symptoms can include a swollen tummy and pain in the back or lower tummy.
Ovarian cancer, fallopian tube cancer and primary peritoneal cancer usually causes symptoms that are similar to common non-cancerous conditions. This can make it difficult to diagnose early. If you have any of these symptoms or get these symptoms regularly, your GP should offer you cancer tests:
- a long-lasting bloated or swollen stomach (tummy)
- feeling full quickly when you eat
- loss of appetite
- pain in the lower tummy area
- back pain
- peeing (passing urine) more often than usual
- needing to pee urgently (feeling like you cannot hold on).
Causes and risk factors of ovarian cancer
We do not know what causes ovarian cancer, fallopian tube cancer or primary peritoneal cancer. There are some risk factors that can increase the chances of developing them.
Age
More than half (50%) of ovarian cancers develop in women after the age of 65. These cancers are rare under the age of 30. The risk of ovarian cancer increases with age.
Hormonal factors
Doctors think the number of times an ovary releases an egg (ovulates) may be linked to ovarian cancer risk. This is because there is evidence that having children, breastfeeding, and taking the contraceptive pill reduces the risk of ovarian cancer.
Hormone replacement therapy (HRT)
Taking HRT, which uses oestrogen, progesterone or both, after the menopause slightly increases the risk of ovarian cancer. About 4 in 100 (4%) of cases may be linked to taking HRT. But doctors think this is only for serous and endometrioid ovarian cancers.
Breast cancer
If you have had breast cancer, you may be more likely to develop ovarian cancer. This may be because these cancer types share the same risk factors. But doctors think it may be because both cancers can be caused by the same cancer genes.
Other conditions
Some other conditions can increase your risk of developing ovarian cancer.
Diabetes
Having diabetes may increase the risk of developing ovarian cancer.
Endometriosis
Endometriosis is a non-cancerous condition. With this condition, cells similar to the cells that line the womb are found in areas outside the womb.
Some people worry about a link between endometriosis and developing ovarian cancer. But studies show that having endometriosis only slightly increases the risk of endometrioid and clear cell ovarian cancers. These types of ovarian cancer are often diagnosed earlier when they are easier to treat successfully.
Lifestyle factors
There are also some lifestyle factors that can increase your risk of developing ovarian cancer.
Weight
Being overweight (obese) may increase the risk of some ovarian cancers.
Smoking
Smoking cigarettes may slightly increase the risk of developing a less common type of ovarian cancer called mucinous cancer. But it does not affect your risk of epithelial ovarian cancer which is the most common type.
Family history of ovarian cancer
Having a family history of ovarian cancer can increase your risk of developing it. If your mother or sister has had ovarian cancer, your risk may be up to 3 times higher. If they were diagnosed at a young age, your risk may be higher.
Your GP can also give you information and support. If they think your family might have an increased risk of ovarian cancer, they may arrange for you to see a genetics specialist.
Inherited genetic conditions
Around 5 to 15 out of 100 (5 to 15%) of ovarian cancers are thought to be caused by a change (mutation) in a gene that is passed on in the family. Genes contain our genetic information, which is passed on from our parents. Some cancers, such as ovarian, breast, bowel and womb cancers, may affect several people in the same family. They may develop at a younger age.
BRCA1 and BRCA2
The most commonly affected genes are called BRCA1 and BRCA2. If you have a mutation in one of these genes, you may have a higher risk of ovarian, fallopian tube, primary peritoneal and some other types of cancer.
Diagnosis of ovarian cancer
Your GP asks about your symptoms and does an internal vaginal examination to check for any lumps or swelling. They usually arrange the following tests:
- a CA125 blood test to check for raised levels of this protein, which may be higher in ovarian cancer
- ultrasound scans to check the organs in the pelvis and tummy area.
If the ultrasound shows any abnormal areas, your GP arranges for you to see a specialist doctor (a gynaecological cancer specialist). You should be seen within 2 weeks.
If a GP finds a lump in your pelvis or fluid in your tummy (ascites), they refer you to a specialist straight away. Sometimes ovarian cancer is diagnosed after being admitted to hospital with a symptom that is making you unwell.
Treatment for ovarian cancer
A team of specialists will meet to discuss the best possible treatment for you. This is called a multidisciplinary team (MDT).
Your cancer doctor and specialist nurse will explain the different treatments and their side effects. They will also talk to you about the things you should consider when making treatment decisions. The main treatments are:
- Surgery: You usually have surgery to remove all or as much of the cancer as possible. It usually involves removing the womb, ovaries and fallopian tubes. If you have a very early stage ovarian cancer you may be able to have surgery to preserve your fertility.
- Chemotherapy: Chemotherapy uses anti-cancer (cytotoxic) drugs to destroy cancer cells. You usually have carboplatin along with paclitaxel. You may have chemotherapy before or after surgery, or both. Sometimes chemotherapy is given on its own as the main treatment if surgery is not possible.
- Targeted therapies: Targeted therapies target something in or around the cancer that is helping it to grow. You may have a type of targeted therapy called a PARP inhibitor drug. You take it as a tablet for as long as it works for you (maintenance treatment).
Click here to learn more about Ovarian Cancer.